Giant mediastinal teratoma in a young infant: a case report
Introduction
Mediastinal masses can present in young infants, the most common of which are thymomas or teratomas. Giant teratomas can pose challenges for resection. In this article we discuss principles for intraoperative management pertaining to anesthesia induction, surgical access, cannulation for cardiopulmonary bypass, and tumor dissection. We present the following case in accordance with the CARE reporting checklist (available at https://med.amegroups.com/article/view/10.21037/med-21-45/rc).
Case presentation
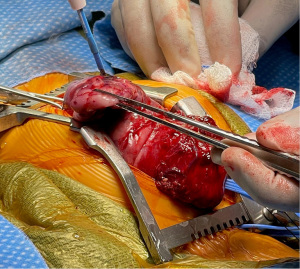
A two-month-old otherwise healthy female child presented to the ER with cough, rhinorrhea, and noisy breathing. Chest X-ray (CXR) showed displaced heart and cystic mass in the mediastinum (Figure 1).
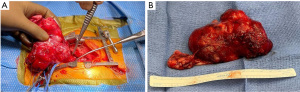
Electrocardiogram (EKG) showed prolonged P waves. Chest CT demonstrated a large mediastinal mass, likely a teratoma (Figure 2).
A transthoracic echocardiogram was performed which confirmed the presence of the mediastinal mass with normal function of the heart, and no obstruction to flow. Pediatric Hematology-Oncology was consulted and alpha-fetoprotein (AFP), ferritin, urine vanillylmandelic acid (VMA) and homovanillic acid (HVA), and ovarian ultrasound were all within normal limits.
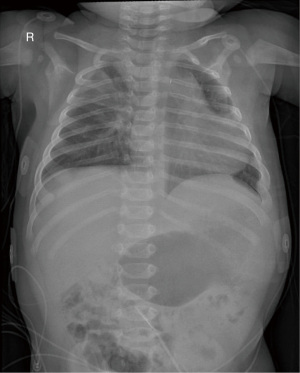
A decision was made to proceed to the operating room for resection of the mediastinal mass. The patient underwent resection of the anterior mediastinal mass on hospital day six. A nasotracheal, deliberate right mainstem intubation was performed without paralysis in light of the risk of cardiovascular collapse and tracheal compression due to the size and location of the mass. Placement of a transesophageal probe was also avoided for the same reason. Preparations were made for urgent sternotomy. Following paralysis, the patient remained hemodynamically stable and attention was turned towards dissection of right neck vessels. The right carotid artery and internal jugular vein were isolated for possible cannulation in case cardiopulmonary support was needed since access to central cannulation (ascending aorta and right atrium) were blocked by the tumor. A standard median sternotomy was then performed. The thymus was noted to be inferiorly displaced and extending to the level of the diaphragm (Figure 3).
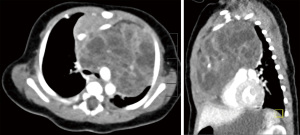
A thymectomy was performed after which the mediastinal mass was clearly visualized. The innominate vein and right internal jugular vein were noted to be severely stretched coursing across the anterior surface of the mass prior to joining with the superior vena cava. The heart was displaced posterioinferiorly and the left lung was displaced laterally. Using a combination of sharp and blunt dissection, separation was initially performed at the superior edge. A plane was developed between the ascending aorta, arch, great vessels, and the mass. Care was taken to avoid injury to the coronary vessels and left phrenic nerve. Following dissection at the aortic isthmus, the mass was finally excised in toto (Figure 4).
A 15-French chest tube was placed in the left chest and anterior mediastinum and the chest was closed. No significant bleeding or arrhythmia complications occurred during the operation. The post-operative course was uncomplicated and the patient was extubated on postoperative day (POD) one. The chest tubes were removed 48 hours later with advancement of feeds and weaning to room air.
A pre-discharge chest X-ray (Figure 5) and echocardiogram showed no structural abnormalities and no pericardial effusion. The patient was stable for discharge home on POD5. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient’s parents for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
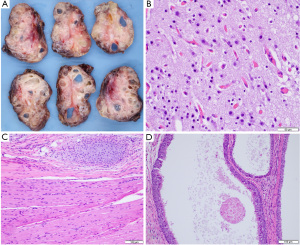
Pathology revealed a heterogeneous solid and cystic tumor (Figure 6A) with one benign lymph node and no areas of immaturity or yolk sac tumor. The mass contained mature elements derived from the three embryological germ cell layers (Figure 6B-6D).
Discussion
In the pediatric population, chest masses are most commonly located in the mediastinum (1). Giant mediastinal tumors can pose unique challenges for resection such as cardiovascular collapse on induction of anesthesia and injury to surrounding structures that may be compressed, displaced, or invaded by the mass (2). Table 1 lists certain principles that must be kept in mind during removal of giant mediastinal masses.
Table 1
| Key points to surgical management of giant mediastinal masses |
| Appropriate cross-sectional imaging to define extent of mass |
| Airway control during anesthesia induction |
| Multidisciplinary collaborative approach including cardiothoracic surgery |
| Preparation for urgent sternotomy |
| Plan for peripheral cannulation to institute cardiopulmonary bypass if needed |
| Preservation of neurovasculature structures during dissection |
| Complete resection whenever possible |
Planning for anesthetic induction is crucial. Selective intubation can be used, especially when there is compression of the lung or distal trachea, such as in our case. Intubation and deep sedation without use of paralytics is desirable. Once intubated, the surgical team should prepare for urgent sternotomy while paralytic agents are administered. If signs of cardiovascular collapse or difficulty in ventilation occur, the surgical team can perform sternotomy, place a stitch over the anterior aspect of the mass and elevate the mass to relieve cardiovascular or respiratory compression that may occur as a result of loss of muscle tone. Involvement of the cardiothoracic surgical team is important when the tumor extensively involves the heart. Preparations should be made to institute peripheral cardiovascular bypass (i.e., neck vessels in small children). Although a plane of dissection can typically be found, one should be prepared for institution of cardiopulmonary bypass in case of extensive encasement or invasion into the heart that precludes access to central cannulation. During dissection, one should proceed from known to unknown areas and develop planes between the mass and surrounding structures. Extraordinary caution should be taken during tumor separation at the proximal aorta where injury to the coronary vessels can occur. Caution should also be exercised during dissection of the isthmus where the ductus arteriosus may be patent and can be injured in infants. It is imperative to safeguard nerves, especially the phrenic and vagus, to the best extent possible. Mature teratomas tend to displace rather than invade nearby structures. The mainstay of treatment is complete excision which results in an excellent prognosis (3). While complete resection is desirable, it may not be achievable especially if the tumor encases coronary arteries, and it is acceptable to leave small amounts of tumor behind (4,5). Following resection, periodic AFP levels and CT should be performed as recommended by the oncology team.
In conclusion, giant mediastinal tumors pose distinct challenges for resection in small infants. The principles of airway control, preparation for urgent sternotomy, preparation for peripheral cardiopulmonary bypass cannulation, and preservation of neurovasculature during dissection must be borne in mind.
Acknowledgments
We would like to thank NYU Langone Hospital for their support.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://med.amegroups.com/article/view/10.21037/med-21-45/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://med.amegroups.com/article/view/10.21037/med-21-45/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient’s parents for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Verma S, Kalra K, Rastogi S, et al. Clinical approach to childhood mediastinal tumors and management. Mediastinum 2020;4:21. [Crossref] [PubMed]
- Li WW, van Boven WJ, Annema JT, et al. Management of large mediastinal masses: surgical and anesthesiological considerations. J Thorac Dis 2016;8:E175-84. [Crossref] [PubMed]
- Kantoff P, Oh W, Shah S, et al. Extragonadal germ cell tumors involving the mediastinum and retroperitoneum [Internet]. 2021 [cited 2021 Aug 6]. Available online: https://www.uptodate.com/contents/extragonadal-germ-cell-tumors-involving-the-mediastinum-and-retroperitoneum#H8
- Goldberg SP, Boston US, Turpin DA, et al. Surgical management of intrapericardial teratoma in the fetus. J Pediatr 2010;156:848-9, 849.e1.
- Minocha P, Hodzic E, Sharma M, et al. Surgical Management of Giant Intrapericardial Teratoma Encasing the Coronary Artery. World J Pediatr Congenit Heart Surg 2022;13:108-10. [Crossref] [PubMed]
Cite this article as: Howell RS, Magid MS, Kuenzler KA, Kumar TKS. Giant mediastinal teratoma in a young infant: a case report. Mediastinum 2022;6:25.