
Non-iatrogenic esophageal trauma: a narrative review
Introduction: anatomy of the esophagus
The esophagus is a muscular tube that traverses three body cavities; the neck, thorax, and abdomen. It sits well protected posteriorly adjacent to the stout and rigid spinal column.
The environment in these spaces is, however different. For example, the thorax, unlike the neck and abdomen, is in a negative pressure space which effects intraluminal pressure dynamics and healing. The pressure gradient from the abdomen to the thorax encourages reflux and will draw enteric contents through an esophageal defect into the pleural space or mediastinum. There are several other unique characteristics to esophageal anatomy that complicate surgical treatment of injury. First, the esophagus has no redundancy thus segmental resections with re-anastomosis are not possible. Second, it has no serosal lining, unlike much of the rest of the gastrointestinal tract (1). Repair of the esophagus can be difficult due to this lack of strength layer. Finally, the esophagus has a relatively poor, segmental blood supply, which if damaged can significantly impair healing of a repaired esophageal injury (2,3). All of these reasons lead to esophageal trauma having a high morbidity and mortality (3). Non-iatrogenic blunt and penetrating trauma to the esophagus are a relatively rare occurrence, compared to iatrogenic trauma (4). The workup and management of non-iatrogenic trauma continues to evolve, with new innovative approaches available for both diagnosis and treatment. The aim of this narrative review is to comprehensively describe the current incidence, presentation, workup, treatment approaches and outcomes of non-iatrogenic esophageal trauma. We present the following article in accordance with the Narrative Review reporting checklist (available at https://med.amegroups.com/article/view/10.21037/med-21-41/rc).
Methods
A thorough literature review was performed using PubMed between January 1, 1960 to September 30, 2021. Full length articles in the English language were included in the review that focused on the epidemiology, workup and treatment of non-iatrogenic esophageal trauma, including current surgical techniques. The search strategy is shown in Table 1.
Table 1
| Items | Specification |
|---|---|
| Date of search (specified to date, month and year) | 15th October 2021 |
| Databases and other sources searched | PubMed |
| Search terms used (including MeSH and free text search terms and filters) | Keywords used: esophageal trauma, non-iatrogenic esophageal trauma, cervical esophageal trauma, abdominal esophageal trauma, thoracic esophageal trauma |
| Timeframe | January 1, 1960 to September 30, 2021 |
| Inclusion and exclusion criteria (study type, language restrictions etc.) | Full length publications available in English |
| Selection process (who conducted the selection, whether it was conducted independently, how consensus was obtained, etc.) | Primary authors conducted selection independently |
Incidence of non-iatrogenic esophageal trauma
The most common causes of full thickness esophageal injury are spontaneous perforation and iatrogenic injury, while non-iatrogenic blunt and penetrating trauma to the esophagus is a relatively rare occurrence (4,5). Among all trauma patients, the incidence those who have of traumatic injuries to the esophagus is low from <1% to 10% (3,6-8).
Injuries to the cervical esophagus are more common than injuries to the thoracic esophagus, with roughly double the amount of cervical esophageal traumatic injuries as compared to thoracic esophageal injuries (9). This is most likely due to the fact that the cervical esophagus is simply less protected due to location.
Demographics
The vast majority—60% to 80%—of patients who present with non-iatrogenic esophageal trauma are young males. The average age of patients with traumatic esophageal injuries is late 20s and early 30s (9,10). There is a disproportionate number of minorities who present with traumatic esophageal injuries, for example one study showed that close to 90% of the patients with esophageal trauma were either black or Hispanic-Americans (11).
Etiology
Globally, penetrating trauma to the esophagus is much more common that blunt (12,13). Of the different types of penetrating trauma, in the United States gunshot wound is the most common form and accounts for 70% to 80% of all esophageal trauma and stab injuries account for 15% to 20% of esophageal traumatic injuries (14,15). Blunt trauma is thought to be the predominant force causing esophageal injury anywhere from 1% to 13% of the time (10,12). Unlike the aorta and proximal airways, the esophagus is not at high risk for trauma from a deceleration injury (16).
There have been various retrospective studies looking at the incidence of blunt and penetrating trauma to the esophagus using different national databases. As might be expected, the etiology of trauma is dependent on the location of the study. In Scotland, where gun ownership is quite low, there is a lower incidence of penetrating esophageal trauma as compared with other countries (8). In Turkey there is a slightly higher incidence of penetrating trauma (17,18). In South Africa, there is a higher incidence of penetrating trauma, more due to knives than firearms (7). In the United States there is a higher incidence of penetrating trauma due to gunshot wounds which are more common than stab wounds (9).
Signs and symptoms
Signs and symptoms of esophageal injury are much less important than the mechanism of injury, and lack of symptoms has a poor negative predictive value. Esophageal injury can present with dysphagia, nausea, hemoptysis, hematemesis, and hoarseness, among other things. One common scenario in a patient with esophageal trauma is pain with swallowing—odynophagia—and difficulty swallowing oral secretions (1). The Mackler Triad—chest pain, vomiting, and subcutaneous emphysema is one constellation of signs and symptoms associated with esophageal injury (3).
Signs to look for with traumatic injury to either the cervical or thoracic esophagus are subcutaneous emphysema, mediastinal ‘crunching’ on auscultation, and stridor (19). However, signs and symptoms which are concerning for an esophageal injury are not indicative of an esophageal injury the vast majority of the time. In a large prospective study there were 98 patients who underwent an esophagogram due to high clinical index of suspicion for esophageal injury due to symptoms or proximity of their external wound to the esophagus, and only two had an esophageal injury (20).
Workup
The most important initial workup for esophageal injuries, is a directed physical exam and high clinical suspicion based on the trajectory or mechanism of injury (9). For unstable patients the principles of advanced cardiac life support (ACLS) must be followed, especially in the case of patients with hemorrhage or an unstable airway, even if an esophageal injury is suspected (21-23). Timing is of the utmost importance for successful management of a traumatic esophageal injury, and any delay can lead to a higher rate of complications and mortality (24,25).
X-ray
If a patient is stable, and there is a penetrating injury which violates the platysma in the neck, there must be suspicion for esophageal injury. Lateral X-ray of the neck, can be used in the trauma bay to look for subcutaneous air outside of the trachea or esophagus when looking for cervical esophageal injury. Chest X-ray can show pneumomediastinum, widened mediastinum, pneumothorax, or pleural effusion. All of these findings should be investigated further to rule out esophageal traumatic injury.
Computed tomography (CT) scan
When an esophageal injury is considered, CT scan of the neck, chest, and abdomen should be obtained in the stable patient. This can help to elucidate the trajectory of a projectile, or help to show radiographic abnormalities which would suggest injury to the esophagus. The Western Trauma Association recommends a CT scan in patients who are hemodynamically stable and have a penetrating neck injury, and for all patients for whom a thoracic esophageal traumatic injury is suspected (19,22). Pneumomediastinum on CT scan should be investigated further in the setting of trauma (3). CT scan combined with esophagography will increase likelihood of a correct diagnosis than if either modality is used alone (26). Another important use of CT scanning is to monitor the progress of a patient who had an esophageal injury to look for signs of complications such as new fluid or air collections outside of the esophagus as the patient progresses during their hospital stay after initial treatment (27).
Esophagography
For patients who are stable, and the index of suspicion for a traumatic esophageal injury is high, a more specific test that can be performed is a contrast esophagography. This is the standard first step in most centers for stable non-intubated patients who are able to swallow (7). Sensitivity for esophageal perforation is 80% to 100% and specificity is 94% to 100% (19). However, for an esophagogram to take place the patient must be awake, able to follow commands, and able to tolerate oral intake. Gastrografin can be used initially due to its lower risk of causing a mediastinitis, and barium can be used afterwards due to its higher diagnostic accuracy (28). One of the main downsides of esophagography is that it can have a false negative rate of 10% to 40% (11). This is especially true in the cervical esophagus where endoscopy is a more reliable diagnostic tool (29). Clinical practice guidelines published in the Journal of Trauma in 2008 state that the use of either contrast esophagography or esophagogastroduodenoscopy (EGD) as an initial diagnostic tool to investigate non-iatrogenic esophageal trauma are equivocal (21).
Endoscopy
Endoscopy has a number of advantages over esophagography in the trauma setting. For one, it can be performed in patients who are intubated, or otherwise unable to follow commands and swallow, as would be needed to perform an esophagram. It can be performed in a number of different settings, including the trauma bay or intensive care unit expeditiously. It can also be performed in the operating room not only to help identify an esophageal injury, but also to help perform a leak test to check the integrity of an esophageal repair. Esophagoscopy has a >90% sensitivity and specificity for identifying an esophageal injury (11). It is more sensitive in the hypopharynx than contrast esophagography (29). EGD can also be combined with contrast such that instillation of water- soluble contrast material through the working channel of the flexible endoscope (even in combination with post-interventional CT-scan) can enhance the diagnostic accuracy considerably.
The downsides of EGD as a diagnostic tool for identifying traumatic injury to the esophagus, is that it is an invasive procedure, with potential complications although the actual number of complications from a diagnostic upper endoscopy is quite low (11). Because esophageal injuries are so rare and use of upper endoscopy has become so routine—the number of EGDs that need to be done to identify a non-iatrogenic traumatic esophageal injury is quite high (30). Although, because the mortality of a traumatic esophageal injury is around 20%, and in some studies has been shown to double if there is a delay in diagnosis many centers favor using EGD for to aid in diagnosis of an esophageal injury if the clinical suspicion is high (31-33).
Surgical exploration as diagnostic tool
Mandatory surgical exploration had once been an important part of the workup for someone with concern for esophageal trauma (34). This was especially the case for cervical penetrating trauma, where it was suggested that surgical exploration should be performed in all patients who had a wound which violated the platysma. However, with the high rate of negative explorations, routine surgical exploration of the neck, especially in asymptomatic patients with imaging and endoscopy findings that are negative has fallen out of favor (21,35).
Cervical esophageal trauma treatment
An algorithm highlighting the approach, workup and management of cervical esophageal trauma is shown in Figure 1.
Observation
For patients with confirmed cervical esophageal trauma, observation alone can be a satisfactory treatment. The extent of the injury will dictate whether this can be done safely. For lower grade injuries, such as contusions, hematomas, or partial thickness laceration, observation is the standard of care. For lacerations of unknown depth, often an esophagram is performed to see if there is leakage of contrast material through the injury. In the cases where there is contrast extravasation, if it is contained and not free flowing there are some centers that advocate observation, and have had reasonable outcomes with this (36,37). In a contemporary large series on esophageal trauma 19% of patients with a confirmed esophageal traumatic injury were treated with observation alone and had acceptable outcomes; this involves a period on nil per os (NPO) between 5 to 7 days followed by esophagram and—if negative—starting a clear liquid diet, followed by diet advancement over the next 1 to 2 weeks (10). There are some guiding principles for the selection of patients for whom one should treat non-operatively. Most important is that the perforation is contained, it is caught within the first 48 hours, there are minimal symptoms, and there are no signs of early or developing sepsis (13).
Debridement and drainage
If cervical neck exploration reveals a cervical esophageal injury which has wound edges that are not clean and easy to identify, debridement and drainage of the area of injury without esophageal repair can be done (7,10). A flat drain is usually placed in the area of the injury which has been debrided, and left it place for several days while the patient is NPO and fed either with a post pyloric feeding tube or with total parenteral nutrition (TPN). Once they have been NPO for several days an esophagogram can be performed to see if the injury has healed. Once it has healed, the drain can be removed, and a diet can slowly be reinstated (7).
Repair
When there is an injury that is identified, either on neck exploration, esophagram, or EGD consideration should be taken to primarily repair a cervical esophageal traumatic injury. Overall, esophageal repair is the most common surgical treatment of traumatic esophageal injury (9,10). In one of the largest series on non-iatrogenic esophageal injury 87% of patients underwent primary esophageal repair (38).
First and foremost is adequate exposure of the site of injury through a lateral neck or cervical collar incision. Extreme care must be taken to avoid injury to the recurrent laryngeal nerves by identification in the tracheoesophageal groove. Certainly, a careful inspection of adjacent structures including the trachea, thyroid and vasculature is important to identify adjacent injuries (39). Mobilization of the esophagus should be as minimal as possible, furthermore, to avoid injury to the segmental blood supply. Once the injury is identified, a key step is to divide the muscular layers of the esophagus above and below the mucosal injury to a point where the entire length of the mucosal injury can be clearly seen. There must be clean healthy edges of mucosa seen and sutured to each other for appropriate closure. Once the distal and proximal extents of the injury are clearly seen, the injury should be closed in two layers (39). The mucosal layer should be closed first, with interrupted sutures taking care not to take too much tissue and cause a stenosis. Next, the muscle layer should be closed over the top of the mucosal repair.
Once the repair is complete, an endoscope can be advanced into the area of the injury and the esophagus can be insufflated while the injury is submerged in saline on the outside. If there are no bubbles that come through the injury, this would be considered a negative leak test which can give reassurance that the injury has been properly repaired.
For additional coverage, when tissue viability is a concern (such as concern for blast injury), a muscle flap buttress can be placed over the cervical esophageal repair (13). The most easily available muscle would be the sternocleidomastoid. This muscle can be detached from either its distal or proximal insertion—due to its dual blood supply, and rotated over to cover a repair site. Other available muscles include the omohyoid or strap muscles. The area of the repair should have a drain placed in proximity. The patient should remain NPO for some period of time between at least 5–10 days afterwards to allow the injury to heal (9).
Esophageal diversion
A rare way to treat a cervical esophageal traumatic injury is with esophageal diversion. If there is an injury which is not able to be repaired, the esophagus can be resected and left in discontinuity (40). The esophagus must be resected above and below the injury. Once the injured portion of the esophagus is resected, the esophageal hiatus is closed and an end esophagostomy is created from the remnant proximal esophagus in the neck. This can be difficult with a cervical esophageal injury. Ideally, if esophageal diversion is performed, there is enough proximal esophagus to make a diverting esophagostomy below the clavicle (40). If inadequate length, the ostomy becomes part of the wound closure. Unfortunately, this is a challenging area to pouch for saliva management.
Thoracic esophageal trauma treatment
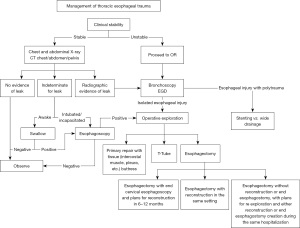
An algorithm highlighting the approach, workup and management of thoracic esophageal trauma is shown in Figure 2.
Observation
Once an injury has been identified in the thoracic esophagus, it must be determined if it is full thickness or not. For low grade injuries, which are not full thickness it is reasonable to observe these patients (41). Maintaining them for a period of time nil per oral and acting quickly if there is any clinical suspicion of progression of injury is necessary. If there is a full thickness injury that is contained, it may be reasonable to observe a patient, however most often full thickness thoracic esophageal injuries must be intervened upon.
Endoscopic therapy
In recent years there has been a movement toward endoscopic therapy of non-iatrogenic esophageal traumatic injuries (42). As advanced endoscopy continues to evolve there are more options for non-iatrogenic thoracic esophageal injuries. For lacerations which are not full thickness, endoscopic clipping with smaller through the scope type clips can be used. For larger injuries, including those that are full thickness, larger over the scope clips can be used for esophageal repair. Recently, the use of vacuum assisted dressings (endo sponge) placement has also been proposed to control extra-luminal sepsis and promoted wound healing, however has the associated complication of bleeding up to 10% of the time. This vacuum system is replaced endoscopically every 48–72 hours until the defect is closed (43).
More commonly, stents are being placed at the site of an esophageal injury (44,45). When they are successful, stents can be a cost effective, less morbid, and well tolerated option for esophageal repair. However, if they are not effective, a traumatic injury which may have initially been able to be repaired may require an esophagectomy—due to prolonged spillage and surrounding soilage—which is much more morbid and has a higher mortality rate than an early esophageal repair (46). To be effective a covered stent must be used. The perforations cannot be greater than 6 cm. Stents are less commonly used in the proximal cervical esophagus due to an uncomfortable globus sensation they can produce. Stents at the gastro-esophageal junction are also less effective because at this location there is a higher risk of stent migration into the stomach or incomplete coverage of an injury at the gastroesophageal (GE) junction.
There is a limited amount of data available regarding stents for traumatic esophageal injury, because it is such a rare occurrence. Based on a recent study, there seems to be a higher risk of leak when patients are treated with an esophageal stent as opposed to esophageal repair, with reported leak rates as high as 80% (10). If a non-iatrogenic thoracic esophageal injury is identified, and stenting is used, the body cavity—usually the pleural space, or mediastinum—which was contaminated by any spillage from the injury must have source control either surgically or with drain placement. When the pleural space needs to be drained surgically, it is reasonable to use a minimally invasive approach such as video-assisted thoracoscopic surgery (VATS). Covered stents have a tendency to migrate, so it is recommended that they are fixed in place either with a clip, endoscopic stitch, or bridle (47). In stenting for esophageal perforation of any kind, the rate of endoscopic reintervention has been reported to be as high as 17% and surgical intervention after stent placement as high as 9.7% (48).
Esophageal repair
The most conventional and common way to treat a non-iatrogenic esophageal injury is with an esophageal repair. The location of the injury will dictate the approach. If the injury is in the proximal to mid thoracic esophagus, a right sided thoracotomy should be performed. If the injury is in the distal thoracic esophagus, a left sided thoracotomy is used. Video assisted approaches either robotic of VATS are not advocated by the authors due to the emergent, time sensitive, and high associated morbidity and mortality involved with non-iatrogenic esophageal trauma. When making a thoracotomy to explore, and potentially repair a thoracic esophageal injury, it may be useful to harvest an intercostal muscle flap on the way in to use for coverage. The repair itself is performed with the same principles in the chest as it is in the neck. All devitalized tissue must be cleared away. The mucosal injury must be fully exposed by dividing esophageal muscle above and below the most proximal and distal areas of the mucosal injury. Once the injury is fully exposed, the mucosal defect should be repaired and the muscle should also be closed above this area. Flap buttress of the repair is advised. If an intercostal muscle flap was taken on the way into the chest this is a good well vascularized option for tissue coverage. Use of pericardium, diaphragm, serratus, latissimus, rhomboid, and thymus have also been described (28). As a last resort, a pleural flap can be developed from the chest wall and draped over the injury; this is known as a Grillo flap (49). The site of the repair should be well drained, and the patient should remain NPO for some time after surgery to give the esophagus time to heal. Even with appropriate repair following all of the guidelines mentioned above, there is a 10–30% incidence of leak after a cervical esophageal repair and 17% after thoracic esophageal repair (37).
Esophagectomy
If there is a substantial injury to the thoracic esophagus, or if there is a delay in diagnosis and it does not look as if the esophagus can be repaired, an esophagectomy can be performed (50,51). The safe and quick salvage operation is esophageal resection, without reconstruction, and with creation of an end cervical esophagostomy. Before this operation is started, feeding access must be considered. A percutaneous endoscopic gastrostomy tube can be placed at the beginning of the case, before the thoracotomy for the esophageal resection. This avoids operating in the abdomen because, at the time of eventual esophageal reconstruction, there will be fewer adhesions.
The side of the thoracotomy will be dictated by the site of the injury, and the site of any signs of pleural contamination. The esophagectomy then requires resection of the distal esophagus past the portion of the esophagus that is injured in the chest. Next, the esophageal hiatus is closed. The rest of the esophagus in the chest is mobilized as high up into the neck as possible. Notably, this dissection is much more commonly performed from the right chest but can be accomplished from the left, similar to the performance of a left-sided thoracoabdominal esophagectomy. If there is significant spillage or infection in the pleural space, this must be fully debrided and drained. Chest tubes are placed for continued wide drainage. Then, after the chest is closed, the patient is transitioned from a lateral position to a supine position, and the proximal esophagus is approached through the neck. An incision is made parallel to the sternocleidomastoid muscle near the sternal notch. The esophagus is dissected out of the space between the trachea and the spine, taking care to avoid injury to the recurrent laryngeal nerve. Once the esophagus is encircled and brought through the cervical incision, it is then tunneled subcutaneously below the level of the clavicle, and brought out through the skin as a cervical end esophagostomy. The authors strongly discourage leaving a blind-ended esophagus with a nasogastric (NG) drain in position unless stability of the patient demands this. This blind stump will rupture within days due to the force of contained esophageal peristalsis despite drainage. If this must be done, plans must be made for operative diversion as soon as medically possible.
Once the patient has stabilized, after a delay of three to six months esophageal reconstruction can be considered. Reconstruction is preferentially performed with a substernal gastric pull up, but can also be performed with a colon or jejunal interposition if the stomach is not available.
T tube
For high grade thoracic esophageal injuries which are not amenable to repair, and for which esophagectomy is too high-risk endeavor due to comorbidities, or other injuries, a T tube can be used. The T tube is placed in to the esophagus with one limb going proximal in the esophagus, one limb going distal in the esophagus, and the draining end coming out of the chest (52). This T tube will stay in place for an extended period of time usually 6−8 weeks. Once the tract around the draining end has matured, and the original injury has healed, the T tube can be removed endoscopically to avoid more trauma to the healing track. Once removed the track that it was coming through closes. In a large meta-analysis, which looked at overall mortality for esophageal repair using a T tube, mortality in those having T tube repair was 20% (51).
Abdominal esophageal trauma treatment
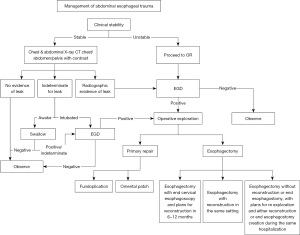
An algorithm highlighting the approach, workup and management of abdominal esophageal trauma is shown in Figure 3. Due to such a short segment of the esophagus being contained in the abdomen, the incidence of abdominal esophageal trauma is lower than that of either the cervical or thoracic esophagus (14,17,30). When an injury is identified in the abdominal esophagus it is most often approached with a laparotomy. If the injury extends to the thoracic esophagus, the hiatus can be opened, in order to visualize the full extent of the injury. If the exposure remains insufficient with this maneuver, a separate thoracotomy can be performed. If the injury is known to be long base on pre-operative workup, a thoracoabdominal incision can also be used from the beginning.
As with the thoracic esophagus, an injury to the abdominal esophagus should be primarily repaired if possible. The site of primary repair should be covered with vascularized tissue. In the abdomen omentum can be used. Additionally, a Nissen fundoplication can also be used. The use of minimally invasive laparoscopic exploration and repair in the setting of non-iatrogenic esophageal trauma is not advocated by the authors.
Associated injuries
Due to the nature of non-iatrogenic trauma and the relatively protected location of the cervical esophagus, injuries of the cervical esophagus will often be affiliated with associated injuries (9). When esophageal injuries are combined with injuries to other organs, it is more likely due to gunshot injury than any other injury due to the deeper penetration that occurs with these (39). The most common associated injury is an injury to the trachea (9). When both the esophagus and the trachea are injured, mortality can double compared with esophageal injury alone (18). When both the esophagus and the trachea have significant injury, the overall morbidity is high, 74% in one large series (39). Complications include trachea-esophageal fistulas, carotid artery rupture, esophageal leaks, and mediastinal abscesses. In order to avoid these potentially devastating complications, when a trauma requires repair of both the esophagus and trachea placing a muscle flap between the repairs is advocated (39).
The next most common associated injury is any injury to major vessels in the neck and the cervical esophagus (9). If both of these structures are damaged enough to require repair, placing a muscle flap between the repairs can help avoid late complications (53). Such complications include carotid artery pseudoaneurysm or carotid artery blow out. Esophageal trauma associated with a major vascular injury will have a higher mortality (54).
Other associated injuries that have been described are injuries to the thyroid, spinal cord, recurrent laryngeal nerve, lung, and thoracic duct (9).
Outcomes
Mortality
The mortality associated with non-iatrogenic trauma to the esophagus is high. Overall mortality in numerous studies place this number between 20% to 70% (8,9,15,55). In a contemporary retrospective review of the National Trauma databank the overall mortality associated with a non-iatrogenic esophageal injury is 14% for thoracic and 8% for cervical injury (6). Mortality is higher in patients with thoracic esophageal trauma as compared with cervical esophageal trauma, with some series showing double the mortality for thoracic esophageal injuries when compared with cervical (3,9). In one large series mortality was highest for thoracic esophageal injuries at 35%, followed by cervical which had a mortality of 15% (38). In the National Trauma Databank study, a higher mortality was associated with thoracic esophageal injury, delay in treatment, a higher grade injury, and older age (6).
When initial presentation is stratified by the Pittsburg Severity Score which is a measurement of the severity of an esophageal perforation the patients with the highest Pittsburgh Severity Score had an 18-fold higher chance of mortality than those with the lower Pittsburgh Severity Score (56). The injury severity score (ISS) is also well correlated with mortality, the higher the ISS the higher the mortality (3). Blunt injury to the cervical esophagus has a reported mortality of 20%, whereas penetrating cervical esophageal injury has a lower mortality at roughly 10% (6,57). Time to treat, from initial presentation to definitive management seems to be one of the most important factors in influencing mortality (9,58). A delay in diagnosis of an esophageal injury can lead to mortality of up to 60% in some series (6,54,59). This is most likely due to an unrecognized sepsis that can occur due to spillage of enteric contents through an esophageal injury. Late mortality is associated with sepsis or fistula formation (9).
Morbidity
Patients who suffer from esophageal trauma, have a high rate of complications, approaching 50% (3). Increased morbidity is seen in patients who have blunt esophageal trauma as compared with penetrating esophageal trauma. Specifically, the incidence of infectious complications and fistula formation is higher in the blunt group as is total hospital length of stay (10). When there is a delay between presentation and surgery, for patients who require an operation, the morbidity has been found to increase (14).
When esophageal trauma has associated injuries in the vicinity of the esophageal injury such as tracheal or carotid injury, the mortality also increases significantly. These associated injuries are a marked of more severe trauma, can be more difficult to fix, and can be associated with late complications.
In patients who are treated with an esophageal repair, the leak rate can be as high as 30% and 40% of patients who had an esophageal repair may need subsequent procedures after their repair (17). Late complications include infection from empyema, abscess, fistula, and esophageal stricture (19).
Conclusions
Non-iatrogenic esophageal trauma is a rare entity that has a high morbidity and mortality. The diagnosis can often be quite challenging, however is critical to perform in a timely manner.
Workup is multimodal and involves a combination of plain radiographs, CT scans, endoscopy and fluoroscopy depending of the stability of the patient and associated injuries. Management depends on location and extent of esophageal injury, and can include observation, debridement and drainage, esophageal diversion, endoscopic approaches or esophagectomy. Experienced multidisciplinary esophageal teams are important for optimal outcomes. These teams include emergency room physicians, thoracic surgeons, general surgeons, otolaryngologists, gastroenterologists, radiologists, and nutritionists.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Simon R. Turner) for the series “Traumatic Injuries of the Mediastinum” published in Mediastinum. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://med.amegroups.com/article/view/10.21037/med-21-41/rc
Peer Review File: Available at https://med.amegroups.com/article/view/10.21037/med-21-41/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://med.amegroups.com/article/view/10.21037/med-21-41/coif). The series “Traumatic Injuries of the Mediastinum” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bryant AS, Cerfolio RJ. Esophageal trauma. Thorac Surg Clin 2007;17:63-72. [Crossref] [PubMed]
- Johnson SB. Esophageal trauma. Semin Thorac Cardiovasc Surg 2008;20:46-51. [Crossref] [PubMed]
- Makhani M, Midani D, Goldberg A, et al. Pathogenesis and outcomes of traumatic injuries of the esophagus. Dis Esophagus 2014;27:630-6. [Crossref] [PubMed]
- Vázquez-Rodríguez JC, Pelet Del Toro NM, García-Rodríguez O, et al. Traumatic esophageal perforation in Puerto Rico Trauma Hospital: A case-series. Ann Med Surg (Lond) 2019;44:62-7. [Crossref] [PubMed]
- Gupta NM, Kaman L. Personal management of 57 consecutive patients with esophageal perforation. Am J Surg 2004;187:58-63. [Crossref] [PubMed]
- Aiolfi A, Inaba K, Recinos G, et al. Non-iatrogenic esophageal injury: a retrospective analysis from the National Trauma Data Bank. World J Emerg Surg 2017;12:19. [Crossref] [PubMed]
- Madiba TE, Muckart DJ. Penetrating injuries to the cervical oesophagus: is routine exploration mandatory? Ann R Coll Surg Engl 2003;85:162-6. [Crossref] [PubMed]
- Skipworth RJ, McBride OM, Kerssens JJ, et al. Esophagogastric trauma in Scotland. World J Surg 2012;36:1779-84. [Crossref] [PubMed]
- Defore WW Jr, Mattox KL, Hansen HA, et al. Surgical management of penetrating injuries of the esophagus. Am J Surg 1977;134:734-8. [Crossref] [PubMed]
- Raff LA, Schinnerer EA, Maine RG, et al. Contemporary management of traumatic cervical and thoracic esophageal perforation: The results of an Eastern Association for the Surgery of Trauma multi-institutional study. J Trauma Acute Care Surg 2020;89:691-7. [Crossref] [PubMed]
- Srinivasan R, Haywood T, Horwitz B, et al. Role of flexible endoscopy in the evaluation of possible esophageal trauma after penetrating injuries. Am J Gastroenterol 2000;95:1725-9. [Crossref] [PubMed]
- Sudarshan M, Cassivi SD. Management of traumatic esophageal injuries. J Thorac Dis 2019;11:S172-6. [Crossref] [PubMed]
- Altorjay A, Kiss J, Vörös A, et al. Nonoperative management of esophageal perforations. Is it justified? Ann Surg 1997;225:415-21. [Crossref] [PubMed]
- Asensio JA, Chahwan S, Forno W, et al. Penetrating esophageal injuries: multicenter study of the American Association for the Surgery of Trauma. J Trauma 2001;50:289-96. [Crossref] [PubMed]
- Patel MS, Malinoski DJ, Zhou L, et al. Penetrating oesophageal injury: a contemporary analysis of the National Trauma Data Bank. Injury 2013;44:48-55. [Crossref] [PubMed]
- Petrone P, Kassimi K, Jiménez-Gómez M, et al. Management of esophageal injuries secondary to trauma. Injury 2017;48:1735-42. [Crossref] [PubMed]
- Eroglu A, Turkyilmaz A, Aydin Y, et al. Current management of esophageal perforation: 20 years experience. Dis Esophagus 2009;22:374-80. [Crossref] [PubMed]
- Onat S, Ulku R, Cigdem KM, et al. Factors affecting the outcome of surgically treated non-iatrogenic traumatic cervical esophageal perforation: 28 years experience at a single center. J Cardiothorac Surg 2010;5:46. [Crossref] [PubMed]
- Biffl WL, Moore EE, Feliciano DV, et al. Western Trauma Association Critical Decisions in Trauma: Diagnosis and management of esophageal injuries. J Trauma Acute Care Surg 2015;79:1089-95. [Crossref] [PubMed]
- Demetriades D, Theodorou D, Cornwell E, et al. Evaluation of penetrating injuries of the neck: prospective study of 223 patients. World J Surg 1997;21:41-7; discussion 47-8. [Crossref] [PubMed]
- Tisherman SA, Bokhari F, Collier B, et al. Clinical practice guideline: penetrating zone II neck trauma. J Trauma 2008;64:1392-405. [Crossref] [PubMed]
- Sperry JL, Moore EE, Coimbra R, et al. Western Trauma Association critical decisions in trauma: penetrating neck trauma. J Trauma Acute Care Surg 2013;75:936-40. [Crossref] [PubMed]
- Tessler RA, Nguyen H, Newton C, et al. Pediatric penetrating neck trauma: Hard signs of injury and selective neck exploration. J Trauma Acute Care Surg 2017;82:989-94. [Crossref] [PubMed]
- Vermeulen BD, van der Leeden B, Ali JT, et al. Early diagnosis is associated with improved clinical outcomes in benign esophageal perforation: an individual patient data meta-analysis. Surg Endosc 2021;35:3492-505. [Crossref] [PubMed]
- Lindenmann J, Matzi V, Neuboeck N, et al. Management of esophageal perforation in 120 consecutive patients: clinical impact of a structured treatment algorithm. J Gastrointest Surg 2013;17:1036-43. [Crossref] [PubMed]
- Terrazas M, Marjon L, Geter M, et al. Esophagography and chest CT for detection of perforated esophagus: what factors influence accuracy? Abdom Radiol (NY) 2020;45:2980-8. [Crossref] [PubMed]
- Kumar B, Shenfine J. Esophageal trauma. Surgery 2011;29:563-7.
- Cheadle GA, Cheadle WG. A Review of "Options in Management of Trauma to the Esophagus" (1982) "Submitted for the Literary Festschrift in Honor of J. David Richardson, MD Am Surg 2021;87:183-7. [Crossref] [PubMed]
- Ahmed N, Massier C, Tassie J, et al. Diagnosis of penetrating injuries of the pharynx and esophagus in the severely injured patient. J Trauma 2009;67:152-4. [Crossref] [PubMed]
- Arantes V, Campolina C, Valerio SH, et al. Flexible esophagoscopy as a diagnostic tool for traumatic esophageal injuries. J Trauma 2009;66:1677-82. [Crossref] [PubMed]
- Flowers JL, Graham SM, Ugarte MA, et al. Flexible endoscopy for the diagnosis of esophageal trauma. J Trauma 1996;40:261-5; discussion 265-6. [Crossref] [PubMed]
- Asensio JA, Berne J, Demetriades D, et al. Penetrating esophageal injuries: time interval of safety for preoperative evaluation--how long is safe? J Trauma 1997;43:319-24. [Crossref] [PubMed]
- Inci I, Ozcelik C, Nizam O, et al. Traumatic oesophageal perforation. Scand Cardiovasc J 1997;31:97-100. [Crossref] [PubMed]
- Insull P, Adams D, Segar A, et al. Is exploration mandatory in penetrating zone II neck injuries? ANZ J Surg 2007;77:261-4. [Crossref] [PubMed]
- Weigelt JA, Thal ER, Snyder WH 3rd, et al. Diagnosis of penetrating cervical esophageal injuries. Am J Surg 1987;154:619-22. [Crossref] [PubMed]
- Melmer PD, Chaconas CE, McCrae AL, et al. Conservative Therapy for Cervical Esophageal Perforation Following Blunt Trauma. Am Surg 2021;87:1518-20. [Crossref] [PubMed]
- Ivatury RR, Moore FA, Biffl W, et al. Oesophageal injuries: Position paper, WSES, 2013. World J Emerg Surg 2014;9:9. [Crossref] [PubMed]
- Symbas PN, Hatcher CR Jr, Vlasis SE. Esophageal gunshot injuries. Ann Surg 1980;191:703-7. [Crossref] [PubMed]
- Feliciano DV, Bitondo CG, Mattox KL, et al. Combined tracheoesophageal injuries. Am J Surg 1985;150:710-5. [Crossref] [PubMed]
- Urschel HC Jr, Razzuk MA, Wood RE, et al. Improved management of esophageal perforation: exclusion and diversion in continuity. Ann Surg 1974;179:587-91. [Crossref] [PubMed]
- Kuppusamy MK, Hubka M, Felisky CD, et al. Evolving management strategies in esophageal perforation: surgeons using nonoperative techniques to improve outcomes. J Am Coll Surg 2011;213:164-71; discussion 171-2. [Crossref] [PubMed]
- Herrera A, Freeman RK. The Evolution and Current Utility of Esophageal Stent Placement for the Treatment of Acute Esophageal Perforation. Thorac Surg Clin 2016;26:305-14. [Crossref] [PubMed]
- Siddiqi S, Schraufnagel DP, Siddiqui HU, et al. Recent advancements in the minimally invasive management of esophageal perforation, leaks, and fistulae. Expert Rev Med Devices 2019;16:197-209. [Crossref] [PubMed]
- Ben-David K, Behrns K, Hochwald S, et al. Esophageal perforation management using a multidisciplinary minimally invasive treatment algorithm. J Am Coll Surg 2014;218:768-74. [Crossref] [PubMed]
- Freeman RK, Herrera A, Ascioti AJ, et al. A propensity-matched comparison of cost and outcomes after esophageal stent placement or primary surgical repair for iatrogenic esophageal perforation. J Thorac Cardiovasc Surg 2015;149:1550-5. [Crossref] [PubMed]
- Persson S, Elbe P, Rouvelas I, et al. Predictors for failure of stent treatment for benign esophageal perforations - a single center 10-year experience. World J Gastroenterol 2014;20:10613-9. [Crossref] [PubMed]
- Oprisanescu D, Bucur D, Sandru V, et al. Endoscopic Treatment of Benign Esophageal Fistulas Using Fully-covered Metallic Esophageal Stents. Chirurgia (Bucur) 2018;113:108-15. [Crossref] [PubMed]
- Dasari BV, Neely D, Kennedy A, et al. The role of esophageal stents in the management of esophageal anastomotic leaks and benign esophageal perforations. Ann Surg 2014;259:852-60. [Crossref] [PubMed]
- Grillo HC, Wilkins EW Jr. Esophageal repair following late diagnosis of intrathoracic perforation. Ann Thorac Surg 1975;20:387-99. [Crossref] [PubMed]
- Sudarshan M, Elharram M, Spicer J, et al. Management of esophageal perforation in the endoscopic era: Is operative repair still relevant? Surgery 2016;160:1104-10. [Crossref] [PubMed]
- Biancari F, D'Andrea V, Paone R, et al. Current treatment and outcome of esophageal perforations in adults: systematic review and meta-analysis of 75 studies. World J Surg 2013;37:1051-9. [Crossref] [PubMed]
- Gill RC, Pal KMI, Mannan F, et al. T-tube placement as a method for treating penetrating oesophageal injuries. Int J Surg Case Rep 2016;28:255-7. [Crossref] [PubMed]
- Losken A, Rozycki GS, Feliciano DV. The use of the sternocleidomastoid muscle flap in combined injuries to the esophagus and carotid artery or trachea. J Trauma 2000;49:815-7. [Crossref] [PubMed]
- Brinster CJ, Singhal S, Lee L, et al. Evolving options in the management of esophageal perforation. Ann Thorac Surg 2004;77:1475-83. [Crossref] [PubMed]
- Symbas PN, Tyras DH, Hatcher CR Jr, et al. Penetrating wounds of the esophagus. Ann Thorac Surg 1972;13:552-8. [Crossref] [PubMed]
- Schweigert M, Sousa HS, Solymosi N, et al. Spotlight on esophageal perforation: A multinational study using the Pittsburgh esophageal perforation severity scoring system. J Thorac Cardiovasc Surg 2016;151:1002-9. [Crossref] [PubMed]
- Søreide JA, Viste A. Esophageal perforation: diagnostic work-up and clinical decision-making in the first 24 hours. Scand J Trauma Resusc Emerg Med 2011;19:66. [Crossref] [PubMed]
- Worman LW, Hurley JD, Pemberton AH, et al. Rupture of the esophagus from external blunt trauma. Arch Surg 1962;85:333-8. [Crossref] [PubMed]
- Shirkey AL, Beall AC Jr, De Bakey ME. Surgical management of penetrating wounds of the neck. Arch Surg 1963;86:955-63. [Crossref] [PubMed]
Cite this article as: Schraufnagel DP, Mubashir M, Raymond DP. Non-iatrogenic esophageal trauma: a narrative review. Mediastinum 2022;6:23.



