
Traumatic sternal fractures: a narrative review
Introduction
Traumatic sternal fractures are found in up to 8% of blunt chest trauma patients and 18% of polytrauma patients with thoracic injuries, amid only sporadic cases secondary to penetrating trauma (1,2). They usually result from a direct blow to the anterior chest wall or forced deceleration. The leading mechanism is motor vehicle collision found in 68% of patients, followed by falls (7.9%), motorcycle injuries (7.9%), pedestrian-struck (3.4%), and cyclist injuries (1.4%) (3). The incidence of sternal fractures in motor vehicle collisions ranges from 3% to 6.8% (4). In civilized society, the introduction of seat belt legislation requiring shoulder restraints has led to an increased incidence of sternal fractures (5). Moreover, the widespread use of computed tomography (CT) scan for trauma evaluation increased the diagnosis of even minor sternal fractures (6).
The morbidity of traumatic sternal fractures is typically determined by their presentation and associated injuries, rather than the fracture itself. Isolated sternal fractures have a lower incidence of cardiorespiratory compromise and more favorable trauma scores. In a review of 1,867 patients from the National Israeli Trauma Registry, Odell et al. found that none of the patients with isolated sternal fracture required endotracheal intubation, pleural tube insertion, or thoracotomy compared to 16.9% of polytrauma patients (7). Isolated sternal fractures are rarely associated with blunt cardiac injury (8) and have a low mortality rate of 0.8% (9). Conversely, polytrauma patients with sternal fractures often have severe associated injuries, with mortality of up to 7.9% (3).
With the increase in the diagnosis of traumatic sternal fractures, it is important for the clinician to understand the clinical significance of these injuries, outline their work up and initial evaluation, and review the treatment strategies available, which is the purpose of the current review. We present the following article in accordance with the Narrative Review reporting checklist (available at https://dx.doi.org/10.21037/med-21-27).
Presentation
Patients with sternal fractures typically present with moderate to severe pain localized to the sternum, exacerbated with coughing or sneezing. Dyspnea may be present and could be a manifestation of an underlying pulmonary contusion or hemopneumothorax. On physical examination, overlying ecchymosis or “seat belt sign” can be encountered. Palpation reveals exquisite tenderness and bony crepitus. Laboratory values are often unremarkable or may reveal elevated cardiac enzymes in patients with concomitant blunt cardiac injury.
A portable CXR is often the first imaging test obtained in the trauma bay and is typically unremarkable in a patient with isolated sternal fracture. Ultrasonography is a rapid and inexpensive tool that can be used to diagnose a sternal fracture and associated injuries (10). The sternal fracture appears as a step-off in the anterior cortex at the site of maximal tenderness, running transversely across the sternum (11).
CT scan remains the gold-standard for diagnosis of sternal fracture and is superior to lateral radiography (12). In a large retrospective study of patients with thoracic trauma, 94% of sternal fractures were visible only on chest CT (6). Furthermore, in patients with traumatic sternal fracture, CT scan detects associated thoracic injuries in over 80% of patients (6). The degree of sternal fracture displacement is not necessarily associated with blunt cardiac injury (13).
Associated injuries and blunt cardiac injury
Initial evaluation of patients with traumatic sternal fractures should follow the same general principles of primary and secondary survey. Most patients with traumatic sternal fractures present with polytrauma and multiple associated injuries, while only 26% exhibit isolated sternal fracture (7). The most common associated injuries include rib fractures, pulmonary contusions, pneumothoraces, mediastinal hematoma, and thoracolumbar vertebral fractures (3,7).
A cardinal point in the evaluation of traumatic sternal fractures is the identification of the rare patient with a blunt cardiac injury (14). The Eastern Association for The Surgery of Trauma released a practice management guideline in 2012 summarizing the available evidence for screening of blunt cardiac injury (15). The reader is referred to this document for review. Briefly, an admission ECG should be performed in all patients in whom blunt cardiac injury is suspected. If the ECG is abnormal, the patient should be admitted for continuous monitoring and consultation with cardiology. In case of a normal ECG, a Troponin I level should be obtained. In patients with both normal ECG and Troponin I level, blunt cardiac injury is ruled out and the patient can be safely discharged from the hospital. For patients with hemodynamic instability or persistent new arrhythmia, an echocardiogram should be obtained (15).
Trans-thoracic echocardiogram is a diagnostic study that can show myocardial wall motion abnormalities that would otherwise not be detected by ECG or elevated cardiac enzymes (16). In addition to its ability to detect blunt cardiac injury, echocardiography can stratify the patients with associated moderate injuries (Injury severity score 6 to 15) into groups of those who need continuous cardiac monitoring and those who do not require close surveillance (16).
Treatment
Most patients that present with isolated sternal fractures are treated conservatively with good results (7-9,17). Adequate analgesia plays an important role to minimize the risk of pulmonary complications (18,19). More recently, sternal fixation has gained popularity to fasten recovery and minimize pain although, the overall quality of the studies that support this approach is poor, with the majority being single-surgeon small series (Table 1).
Table 1
| Author | Year | N | Indication | Implant-related complications | Mortality (%) | Mean f/u | Outcomes |
|---|---|---|---|---|---|---|---|
| Al-Qudah (20) | 2006 | 4 | Acute fx. | None | 0 | NR | Healing in all cases |
| Richardson (21) | 2007 | 35 | Acute fx. and nonunion | 1 hardware removal for clicking | 2.8% | NR | Decreased narcotic use. Healing in all cases |
| Ciriaco (22) | 2009 | 6 | Acute fx. | None | 0 | 2–7 yr. | Healing in all cases |
| Divisi (23) | 2011 | 11 | Acute fx. | None | 0 | NR | Healing in all cases |
| Gloyer (24) | 2011 | 3 | Acute fx. and nonunion | 0 | NR | Healing in all cases | |
| Queitsch (25) | 2011 | 12 | Acute fx. and nonunion | 1 wound infection, 1 hardware removal for painful scar | 0 | NR | Healing in all cases |
| Schulz-Drost (26) | 2014 | 10 | Acute fx. | None | 0 | 3 mo. | Healing in all cases |
| Schulz-Drost (27) | 2016 | 3 | Acute fx. | None | 0 | 3 mo. | Healing in all cases |
| Krinner (28) | 2017 | 11 | Acute fx. | None | 0 | 3 mo. | Healing in all cases |
| Zhao (29) | 2017 | 64 | Acute fx. and nonunion | None | 0 | 6 mo. | Decreased pain severity score and improved spirometry |
| Kalberer (30) | 2020 | 15 | Acute fx. | 3 implant removals due to irritation | 0 | 3 mo. | No difference in activities of daily living |
| Bauman (31) | 2021 | 13 | Acute fx. | None | 0 | NR | Decreased pain severity score and narcotic use |
*, all studies are retrospective. Case reports are excluded. F/u, follow up; fx., fracture; N, number of patients; NR, not reported; yr., year(s); mo., months.
Indications for operative fixation of sternal fractures
Currently, there are no published guidelines to make recommendations on operative fixation for sternal fractures. This is probably related to the lack of high-quality evidence in published literature along with patient heterogeneity. In the acute setting, a few studies have shown some improvement in narcotic use and decrease pain severity scores following sternal plating (21,29,31). When malunion or non-union occurs as a delayed complication, surgical stabilization has shown to accomplish sternal healing in most cases (21,24,25,29,31). In summary, surgery should be considered in patients who have unstable fractures, severe displacement or subluxation, symptomatic malunion or non-union (25,29,30).
Surgical technique
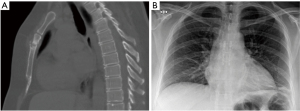
The first description of fixation for a sternal fracture was done in 1943 by McKim (32). Over the last several years, multiple reports have been published regarding different fixation materials including stainless steel wires (33), absorbable plates (34), non-absorbable plates (25,29,30)), and internal cemented screws (35). The most accepted technique involves using titanium plates and screws for plate osteosynthesis (Figure 1), primarily based on data extrapolated from biomechanical testing (36,37) and clinical studies on sternal closure techniques (38,39). A metanalysis by Harston (40) of 12 articles and 76 patients with traumatic sternal fractures (plates were used in 52 patients and wiring in 24 patients), showed healing in all patients regardless of the technique however, sternal plates had a higher removal rate of 15.4%. This finding has not been consistent in more recent studies that are summarized in Table 1.
Most surgeons advocate for an open repair; however, a minimally invasive approach has been described (41). Sternal stabilization after nonunion can be combined with different constituents to aid in fracture healing and restore bone integrity, such as autologous bone grafting (42), synthetic parathyroid hormone (Teriparatide) (43,44) or bone morphogenetic protein (45).
Surgical outcomes
Clinical outcomes after sternal plating for traumatic sternal fractures are difficult to define given that most of the studies are case reports (42-48) and small retrospective series which are summarized in Table 1. In two retrospective studies, plate osteosynthesis was shown to have an acceptable morbidity rate of 0–18% with no evidence of recurrence or hardware failure (25,29). One of the larger series from Zhao et al. (29) of 64 patients with acute fracture and non-union showed decreased pain severity scores and healing in all cases, with a 6 month follow up. Christian et al. (49) queried the Trauma Quality Improvement Program database for patients with sternal fractures (n=9,460) and found that 1.2% of patients underwent surgical stabilization (n=114). They found lower mortality in the surgical group (2.7% vs. 11.2%, P=0.008) but increased median length of stay and ventilator days. There was no difference in the incidence of pulmonary complications after propensity score matching (49). Choi and colleagues (50) analyzed the 2016 National Trauma Data Bank for patients with traumatic sternal fractures after blunt trauma (n=14,760) and found surgical stabilization was performed in 1.8% of patients (n=270). They also found decreased odds of mortality, but no difference in pulmonary complications (50).
A recent metanalysis of 16 studies including 191 patients over recent decades showed a 98% healing rate of sternal fracture following surgical fixation with only a 2% morbidity rate (51). The authors recognized that the overall quality of the studies was poor, with significant methodological and publication bias. Further studies are needed to define the indications and outcomes of surgical stabilization of traumatic sternal fractures.
Complications
Patients with sternal fractures can present with complications related to the fracture itself or its associated injuries. Acute intrinsic complications are rare, such as pericardial impingement, but can be seen with severely displaced fractures (52). Delayed complications of sternal fractures include malunion or non-union (25,33,43-46,48), infection (47,53), and chronic pain (48).
There is no unified definition of sternal fracture nonunion, yet the diagnosis can be made when patients have a persistent fracture without evidence of healing for greater than 3–6 months (33,46). Patients often present with chronic pain exacerbated by deep inspiration or coughing (48). The diagnosis is clinical with physical exam often eliciting pain and clicking at the sternal fracture. When the diagnosis is not clear or the body habitus obscures physical exam, advanced imaging may be obtained (Figure 1). Malunion occurs when the sternal fracture heals in an abnormal position. Patients often complain of a step off at the site of the fracture without clicking.
Chronic pain, symptomatic malunion, and nonunion are the most common indications for operative repair. These recommendations are based on expert opinion and there is no consensus regarding optimal timing from injury. The aims of surgery are to restore the damaged bone surrounding the fracture, stabilize the sternum, manage bone gap if present, and stimulate bone healing.
Sternal infection following trauma is rare (47,53) but is associated with significant morbidity and is treated in a similar fashion to sternal wound infections of other etiologies. The management of sternal wound infections is beyond the scope of this work and is reviewed elsewhere.
Conclusion
Traumatic sternal fractures are rare, with two distinct clinicopathologic entities with different prognosis and management. Isolated sternal fractures are commonly benign injuries that can be managed conservatively in an outpatient setting. Polytrauma patients with sternal fractures should be carefully screened for associated injuries. Surgical stabilization of sternal fractures is feasible and safe, and should be considered in unstable fractures, severe displacement, symptomatic malunion or non-union.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Simon R. Turner) for the series “Traumatic Injuries of the Mediastinum” published in Mediastinum. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://dx.doi.org/10.21037/med-21-27
Peer Review File: Available at https://dx.doi.org/10.21037/med-21-27
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/med-21-27). The series “Traumatic Injuries of the Mediastinum” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Knobloch K, Wagner S, Haasper C, et al. Sternal fractures occur most often in old cars to seat-belted drivers without any airbag often with concomitant spinal injuries: clinical findings and technical collision variables among 42,055 crash victims. Ann Thorac Surg 2006;82:444-50. [Crossref] [PubMed]
- Brookes JG, Dunn RJ, Rogers IR. Sternal fractures: a retrospective analysis of 272 cases. J Trauma 1993;35:46-54. [Crossref] [PubMed]
- Oyetunji TA, Jackson HT, Obirieze AC, et al. Associated injuries in traumatic sternal fractures: a review of the National Trauma Data Bank. Am Surg 2013;79:702-5. [Crossref] [PubMed]
- Khoriati AA, Rajakulasingam R, Shah R. Sternal fractures and their management. J Emerg Trauma Shock 2013;6:113-6. [Crossref] [PubMed]
- Budd JS. Effect of seat belt legislation on the incidence of sternal fractures seen in the accident department. Br Med J (Clin Res Ed) 1985;291:785. [Crossref] [PubMed]
- Perez MR, Rodriguez RM, Baumann BM, et al. Sternal fracture in the age of pan-scan. Injury 2015;46:1324-7. [Crossref] [PubMed]
- Odell DD, Peleg K, Givon A, et al. Sternal fracture: isolated lesion versus polytrauma from associated extrasternal injuries--analysis of 1,867 cases. J Trauma Acute Care Surg 2013;75:448-52. [Crossref] [PubMed]
- Dua A, McMaster J, Desai PJ, et al. The Association between Blunt Cardiac Injury and Isolated Sternal Fracture. Cardiol Res Pract 2014;2014:629687. [Crossref] [PubMed]
- Potaris K, Gakidis J, Mihos P, et al. Management of sternal fractures: 239 cases. Asian Cardiovasc Thorac Ann 2002;10:145-9. [Crossref] [PubMed]
- Racine S, Drake D. BET 3: Bedside ultrasound for the diagnosis of sternal fracture. Emerg Med J 2015;32:971-2. [Crossref] [PubMed]
- Nickson C, Rippey J. Ultrasonography of sternal fractures. Australas J Ultrasound Med 2011;14:6-11. [Crossref] [PubMed]
- Kim EY, Yang HJ, Sung YM, et al. Sternal fracture in the emergency department: diagnostic value of multidetector CT with sagittal and coronal reconstruction images. Eur J Radiol 2012;81:e708-11. [Crossref] [PubMed]
- Heidelberg L, Uhlich R, Bosarge P, et al. The Depth of Sternal Fracture Displacement Is Not Associated With Blunt Cardiac Injury. J Surg Res 2019;235:322-8. [Crossref] [PubMed]
- Laurence G, Grim R, Bell T, et al. The impact of seatbelt use and airbag deployment on blunt thoracic aortic injury. Am Surg 2013;79:E335-6. [Crossref] [PubMed]
- Clancy K, Velopulos C, Bilaniuk JW, et al. Screening for blunt cardiac injury: an Eastern Association for the Surgery of Trauma practice management guideline. J Trauma Acute Care Surg 2012;73:S301-6. [Crossref] [PubMed]
- Wiener Y, Achildiev B, Karni T, et al. Echocardiogram in sternal fracture. Am J Emerg Med 2001;19:403-5. [Crossref] [PubMed]
- Velissaris T, Tang AT, Patel A, et al. Traumatic sternal fracture: outcome following admission to a Thoracic Surgical Unit. Injury 2003;34:924-7. [Crossref] [PubMed]
- Thomas KP, Sainudeen S, Jose S, et al. Ultrasound-Guided Parasternal Block Allows Optimal Pain Relief and Ventilation Improvement After a Sternal Fracture. Pain Ther 2016;5:115-22. [Crossref] [PubMed]
- Appelboam A, McLauchlan CA, Murdoch J, et al. Delivery of local anaesthetic via a sternal catheter to reduce the pain caused by sternal fractures: first case series using the new technique. Emerg Med J 2006;23:791-3. [Crossref] [PubMed]
- Al-Qudah A. Operative treatment of sternal fractures. Asian Cardiovasc Thorac Ann 2006;14:399-401. [Crossref] [PubMed]
- Richardson JD, Franklin GA, Heffley S, et al. Operative fixation of chest wall fractures: an underused procedure? Am Surg 2007;73:591-6; discussion 596-7. [Crossref] [PubMed]
- Ciriaco P, Casiraghi M, Negri G, et al. Early surgical repair of isolated traumatic sternal fractures using a cervical plate system. J Trauma 2009;66:462-4. [Crossref] [PubMed]
- Divisi D, Crisci R. Use of demineralized bone matrix and plate for sternal stabilization after traumatic dislocation. Gen Thorac Cardiovasc Surg 2011;59:52-6. [Crossref] [PubMed]
- Gloyer MA, Frei HC, Hotz TK, et al. Osteosynthesis of traumatic manubriosternal dislocations and sternal fractures with a 3.5/4.0 mm fixed-angle plate (LCP). Arch Orthop Trauma Surg 2011;131:1261-6. [Crossref] [PubMed]
- Queitsch C, Kienast B, Voigt C, et al. Treatment of posttraumatic sternal non-union with a locked sternum-osteosynthesis plate (TiFix). Injury 2011;42:44-6. [Crossref] [PubMed]
- Schulz-Drost S, Mauerer A, Grupp S, et al. Surgical fixation of sternal fractures: locked plate fixation by low-profile titanium plates--surgical safety through depth limited drilling. Int Orthop 2014;38:133-9. [Crossref] [PubMed]
- Schulz-Drost S, Oppel P, Grupp S, et al. The oblique fracture of the manubrium sterni caused by a seatbelt--a rare injury? Treatment options based on the experiences gained in a level I trauma centre. Int Orthop 2016;40:791-8. [Crossref] [PubMed]
- Krinner S, Grupp S, Oppel P, et al. Do low profile implants provide reliable stability in fixing the sternal fractures as a "fourth vertebral column" in sternovertebral injuries? J Thorac Dis 2017;9:1054-64. [Crossref] [PubMed]
- Zhao Y, Yang Y, Gao Z, et al. Treatment of traumatic sternal fractures with titanium plate internal fixation: a retrospective study. J Cardiothorac Surg 2017;12:22. [Crossref] [PubMed]
- Kalberer N, Frima H, Michelitsch C, et al. Osteosynthesis of sternal fractures with double locking compression plate fixation: a retrospective cohort study. Eur J Orthop Surg Traumatol 2020;30:75-81. [Crossref] [PubMed]
- Bauman ZM, Yanala U, Waibel BH, et al. Sternal fixation for isolated traumatic sternal fractures improves pain and upper extremity range of motion. Eur J Trauma Emerg Surg 2021; Epub ahead of print. [Crossref] [PubMed]
- McKim LH. A method of fixation for fractures of the sternum. Ann Surg 1943;118:158-60. [Crossref]
- Wu LC, Renucci JD, Song DH. Sternal nonunion: a review of current treatments and a new method of rigid fixation. Ann Plast Surg 2005;54:55-8. [Crossref] [PubMed]
- Ahmad K, Katballe N, Pilegaard H. Fixation of sternal fracture using absorbable plating system, three years follow-up. J Thorac Dis 2015;7:E131-4. [PubMed]
- Poussot B, Deschamps F, Varin F, et al. Percutaneous Fixation by Internal Cemented Screws of the Sternum. Cardiovasc Intervent Radiol 2020;43:103-9. [Crossref] [PubMed]
- Cohen DJ, Griffin LV. A biomechanical comparison of three sternotomy closure techniques. Ann Thorac Surg 2002;73:563-8. [Crossref] [PubMed]
- Ozaki W, Buchman SR, Iannettoni MD, et al. Biomechanical study of sternal closure using rigid fixation techniques in human cadavers. Ann Thorac Surg 1998;65:1660-5. [Crossref] [PubMed]
- Raman J, Lehmann S, Zehr K, et al. Sternal closure with rigid plate fixation versus wire closure: a randomized controlled multicenter trial. Ann Thorac Surg 2012;94:1854-61. [Crossref] [PubMed]
- Allen KB, Thourani VH, Naka Y, et al. Randomized, multicenter trial comparing sternotomy closure with rigid plate fixation to wire cerclage. J Thorac Cardiovasc Surg 2017;153:888-896.e1. [Crossref] [PubMed]
- Harston A, Roberts C. Fixation of sternal fractures: a systematic review. J Trauma 2011;71:1875-9. [Crossref] [PubMed]
- Xie ZX, Zhou XT, Zhang DS, et al. Minimally invasive plate osteosynthesis for the treatment of sternal fracture in the lower chest: a case report. J Int Med Res 2019;47:4033-8. [Crossref] [PubMed]
- Ebraheim NA, Shafiq Q, Liu J. Nonunion of comminuted transverse sternal fracture involving manubrio-sternal joint fixed with metal plates and autogenous bone graft. J Trauma 2007;62:227-30. [Crossref] [PubMed]
- Marin F. Treatment of Chronic Nonunion of a Sternal Fracture With Teriparatide. Ann Thorac Surg 2021;111:e41-2. [Crossref] [PubMed]
- Chintamaneni S, Finzel K, Gruber BL. Successful treatment of sternal fracture nonunion with teriparatide. Osteoporos Int 2010;21:1059-63. [Crossref] [PubMed]
- Morgan A. Treatment of chronic nonunion of a sternal fracture with bone morphogenetic protein. Ann Thorac Surg 2008;85:e12-3. [Crossref] [PubMed]
- Hendrickson SC, Koger KE, Morea CJ, et al. Sternal plating for the treatment of sternal nonunion. Ann Thorac Surg 1996;62:512-8. [Crossref] [PubMed]
- Rehring TF, Winter CB, Chambers JA, et al. Osteomyelitis and mediastinitis complicating blunt sternal fracture. J Trauma 1999;47:594-6. [Crossref] [PubMed]
- Gallo DR, Lett ED, Conner WC. Surgical repair of a chronic traumatic sternal fracture. Ann Thorac Surg 2006;81:726-8. [Crossref] [PubMed]
- Christian AB, Grigorian A, Nahmias J, et al. Comparison of surgical fixation and non-operative management in patients with traumatic sternum fracture. Eur J Trauma Emerg Surg 2020; Epub ahead of print. [Crossref] [PubMed]
- Choi J, Khan S, Syed M, et al. Early National Landscape of Surgical Stabilization of Sternal Fractures. World J Surg 2021;45:1692-7. [Crossref] [PubMed]
- Klei DS, de Jong MB, Öner FC, et al. Current treatment and outcomes of traumatic sternal fractures-a systematic review. Int Orthop 2019;43:1455-64. [Crossref] [PubMed]
- Tiwari S, Singh A, Bhandari P, et al. Complex open sternal fracture with impingement of the pericardium. Trop Doct 2021;51:425-7. [Crossref] [PubMed]
- Randell PA, Somers L. Case of the month: "bugs are eating my soul"--sternal abscess, osteomyelitis, and mediastinitis complicating a closed sternal fracture. Emerg Med J 2006;23:736-7. [Crossref] [PubMed]
Cite this article as: Doyle JE, Diaz-Gutierrez I. Traumatic sternal fractures: a narrative review. Mediastinum 2021;5:34.


