
Blunt cardiac trauma: a narrative review
Introduction
Trauma is one of the most common presentations to the healthcare system and is a significant contributor to morbidity and mortality. Additionally, trauma is one of the leading causes of disability and death in people under the age of 45 worldwide (1-12). Cardiac trauma is a relatively less common consequence of blunt injury, occurring in less than 10% of trauma admissions; however, it is associated with high rates of morbidity and mortality. Approximately 25% of traumatic deaths occur due to cardiac related injuries (2,8-10,12-15).
Blunt cardiac trauma (BCT) often occurs due to forceful impact, rapid deceleration, or crush injuries without penetration of the chest and heart. The most common causes of BCT include motor vehicle accidents (MVA) (~50% of BCT), pedestrians being struck by a motor vehicle (~35%), motorcycle crashes (~9%), and falls from a significant height. As BCT occurs in the context of great forces on the body, approximately 70–80% of patients with significant BCT have other injuries. The most common comorbid injuries include damage to the brain (42–54%), aorta (47–49%), lung (44–46%), rib or sternum (26–97%), and spine (37%) (1,2,4,7,16,17).
While BCT is certainly an important condition with significant clinical implications, the current literature is limited. There have been few prospective or retrospective studies in recent years and the vast majority of the literature regarding BCT is comprised of case reports and case series. BCTs are often complex cases with various presentations, comorbid injuries, diagnostic modalities, and treatments. Optimal approaches to patients with BCT have not been standardized or widely implemented potentially resulting in sub-optimal outcomes for patients. This review aims to summarize the current literature regarding BCT, the mechanism of injury, presentations, diagnostic and treatment approaches in order to provide an up to date perspective and to identify the areas requiring further investigation in this field. We present the following article in accordance with the Narrative Review Reporting Checklist (available at https://dx.doi.org/10.21037/med-21-19).
Methods
PubMed was searched for English articles published from January 1, 1985 to February 1, 2021. The search terms used to identify relevant articles during screening included “blunt cardiac trauma, blunt thoracic trauma, cardiac trauma, chest trauma, cardiac injury, cardiac contusions, heart valve, heart valve injury, coronary artery injury, aortic injury, free wall rupture, hemopericardium, pericardial injury, and commotio cordis” individually or in combination. Article types included in the search criteria were retrospective, prospective, randomized control trial, case report studies, and previous related reviews. Exclusion criteria included if the full length manuscript was not available and if insufficient data was provided regarding the patient outcomes or the case presented in case reports.
Types of blunt cardiac trauma
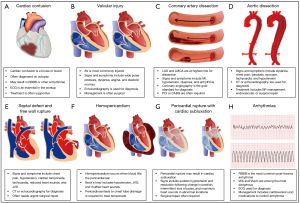
Illustrations and key points for examples of the following injuries have been included in Figure 1.
Cardiac contusions
Cardiac contusions are the most common injuries to the heart resulting from blunt trauma. Mild cardiac contusions often recover without lasting consequences while severe injuries more often result in lasting consequences and mortality (3,6,8,18,19). Signs and symptoms of cardiac contusions include chest pain, shortness of breath, and the development of arrhythmias. While it is commonly stated that cardiac contusion and other cardiac injuries due to blunt trauma are rare, it is hypothesized that this is due to many cardiac contusions being missed or misdiagnosed. Cardiac contusions are often difficult to accurately diagnose due to the lack of standardized approaches to their evaluation. Cardiac contusions also often present with similar symptoms to other more common conditions such as myocardial infarction (MI), often present with comorbid injuries, and may not be high on a differential diagnosis at initial presentation as they are uncommon. The literature remains controversial on the seriousness of cardiac contusions, ranging from benign to life-threatening (3,6,8,18,20-22).
Massive compression of the anterior chest and rapid deceleration are common causes of cardiac contusions. The most common injuries associated with cardiac contusions include MVA, pedestrian struck by motor vehicle, and fall from a height (5,6,20). Since cardiac contusion defines a wide range of injuries, patients may have a variety of presentations. Patients have presented with cardiac contusions ranging from being completely asymptomatic to experiencing mild chest soreness, presenting with electrocardiographic abnormalities, contractile abnormalities, and having signs of heart failure (3,18,23,24).
Right bundle branch block (RBBB) is a common result of cardiac contusions identified in the literature, while left bundle branch block (LBBB) has rarely been reported. The right ventricle is nearest to the sternum, subjecting it to the high risk of cardiac contusions (5). Cardiac contusions can also increase the likelihood of other arrhythmias, low cardiac output, ventricular or free wall rupture, and valvular dysfunction (9,20).
Valvular injuries
Injury to the heart valves is a rare consequence of blunt trauma to the thorax. Out of the 4 valves, the aortic valve (AV) is generally considered to be at the greatest risk for injury, followed by the mitral valve (MV), tricuspid valve (TV), and the pulmonary valve (PV) (1,4,5,9,19,25-32). Although, in a review of more than 1 million hospital discharges, Ismailov et al. documented the incidence of heart valve injuries. Among the included patients they found that incidence of valvular injuries associated with BCT includes 1.25% MV, 0.93% AV, 0.13% TV, and 0.02% PV (33). The left-sided valves are thought to be at higher risk due to increased pressure on the left side of the heart (1,4,5,9,19,25-32). AV injuries include damage to the leaflets, aorta, and coronary arteries. Injuries to the MV and TV may also have involvement of papillary muscle and chordae tendineae. One of the proposed mechanisms of valvular injury during BCT is a blowout of the valve by sudden increased intracardiac pressure against a closed valve (5,9,20,22,25,29,33-35). Injuries commonly associated with valvular lesions include myocardial contusions, atrial septal defect (ASD), ventricular septal defect (VSD), pericardial lesions, cardiac tamponade, coronary artery dissection, aortic dissection, aortic transection, and venous sinus injury (19,36-38).
Diagnosing valvular pathology as a consequence of BCT is often challenging with variable signs and symptoms, significant overlap between the presentation of the different valve injuries, and inconsistent or delayed presentation. For example, signs and symptoms of acute aortic regurgitation (AR) include dyspnea, angina, a wide pulse pressure, and diastolic murmur on auscultation. While signs of acute traumatic mitral regurgitation (MR) include dyspnea, pulmonary edema, fatigue, and murmurs on auscultation, although murmurs may not be audible with severe MR after left ventricular (LV) and left atrial (LA) pressures equalize (20,35,39). Symptoms of MV injury can often have an insidious onset occurring 1 to 2 weeks after injury. In contrast, TV injuries can present with similar signs and symptoms as well as an elevated jugular venous pressure (JVP) with significant V waves but may take months to years for symptoms to develop (1,5,19,20,29).
Coronary artery injuries
A relatively rare cause of death in BCT is coronary artery dissection or rupture occurring in approximately 2–12% of already rare BCT injuries. The most common cause of coronary injury is BCT due to compression between the sternum and spine or rapid deceleration. Due to their positioning posterior to the sternum, the left anterior descending (LAD) and left main coronary artery (LMCA) are at the highest risk of injury and account for approximately 76% of all coronary injuries. The right coronary artery (RCA) is the next most commonly injured coronary at approximately 12% of coronary injuries, and the left circumflex artery is rarely injured. Coronary artery dissection or rupture may result in MI if left untreated (5,9,15). It is believed that existing coronary artery disease (CAD) increases the risk of dissection or rupture. As the LAD is the most commonly injured artery, infarction is most likely to impact the anterior wall of the LV, apex, or septum (1,2,5,7,40).
Coronary artery injury may present with MI or non specific symptoms such as hypotension, dyspnea, and ventricular arrhythmias. Rupture of a coronary artery may lead to rapid cardiac tamponade, leading to death on the scene of the trauma. Diagnosing coronary artery injuries most commonly occur through radiologic investigations which may be delayed in the context of severe trauma (5,9,15,41).
Aortic injuries
Approximately 48% of patients with BCT have an associated thoracic aorta injury (2,19,25). Symptoms of aortic injury include dyspnea, chest pain, paralysis, and syncope (22,42). AV injury is commonly associated with aortic injuries. The most common causes of thoracic aortic injury in blunt trauma include rapid deceleration, compression, and shearing forces against points of fixation such as the ligamentum arteriosum. Common mechanisms of injury include motor vehicle accidents, bicycle accidents, and falls from a significant height (4,14,20,40,43,44).
The aortic isthmus is the most commonly injured location of the aorta as it sits between the fixed aortic arch and descending thoracic aorta leaving it vulnerable to twisting or shearing motions (1,4,5,14,20,43,44). Many patients die of vessel rupture and rapid exsanguination (1). Aortic transection and free rupture caused by horizontal deceleration are associated with mortalities greater than 80% within the first 30 minutes of injury and with a total mortality rate of 75–90% making diagnosis and treatment for these patients impossible. Victims of aortic dissection that do not die on the scene often have their aorta contained within a thin layer of the intima. These patients may present to hospital but their risk of subsequent rupture is high, with up to 50% mortality within 7 days if left untreated (12,14,20,41,45).
Septal defects and free wall ruptures
Cardiac rupture can occur in the atrial septum, ventricular septum, or a free wall of the heart. Rupture of one or more of the cardiac chambers is a highly lethal event with death often occurring at the scene of the trauma. Common causes of injury include MVA, pedestrians struck by motor vehicles, or falls from significant heights. The most commonly injured cardiac chamber is the right ventricle (RV), followed by the right atrium (RA), left ventricle (LV), and left atrium (LA). Atrial injuries are often at the venous-atrial confluence with injuries at the junctions of the inferior vena cava (IVC) and RA, and pulmonary veins and LA being relatively common. Atrial injuries are also more common when the atrioventricular valves are closed in late systole, while injuries occurring in end-diastole as maximal filling of the ventricles is more likely to result in ventricular rupture (1,2,4,6-9,20,23,27,30,34,41,46-51).
Signs and symptoms of septal or free wall rupture often vary based on the location of the rupture making initial identification difficult. The patients who survive to presentation are more likely to have septal rupture or atrial free wall rupture as the atria are lower pressure chambers, therefore taking more time to develop cardiac tamponade. These patients often present with non-specific signs of chest pain, hypotension, cardiac tamponade, elevated central venous pressure, tachycardia, unresponsiveness, reduced heart sounds, jugular venous distention, and increased heart shadow size on CXR (1,6,8,20,52,53).
A traumatic VSD can form in both the membranous and muscular portions of the septum. With a free wall rupture, if the ruptured myocardium is sealed off by the pericardium and thrombus, a pseudoaneurysm can develop, which itself has a high risk of rupture (1,27,30).
Hemopericardium and pericardial injuries
Blunt pericardial injury is a rare condition. Common causes involve high energy impact or high abdominal pressures and include MVA and fall from significant heights (1,4,22,54-57).
There are several consequences of trauma that may involve the pericardium, although they are rare in blunt trauma relative to other injuries. These include pneumopericardium, hemopericardium, pleural effusion, cardiac tamponade, pericardial rupture which can result in cardiac subluxation if large enough, and delayed constrictive pericarditis (2,54). Common sites for pericardial rupture include the diaphragmatic pericardium and pleuropericardium. A diaphragmatic pericardial rupture may result in abdominal contents herniating into the pericardium. Conversely, if the pleuropericardium is ruptured, the heart may herniate out of the pericardial sac and into the pleural space (4,58). Hemo and pneumopericardium occur when the pericardial sac fills with blood or air, respectively. Cardiac tamponade occurs when the fluid in the pericardium creates a pressure equal to or greater than the pressure in the chambers of the heart preventing filling and output to and from the heart with a significant drop in systolic blood pressure. Tamponade often occurs acutely with blunt traumatic injury, cardiac contusions, or rupture and can occur with as little as 200mL of fluid. There are cases of patients experiencing delayed hemopericardium days or weeks after the trauma they experienced (34,59,60).
Signs and symptoms of pericardial injury may include chest pain, tachycardia, dyspnea, and hyper or hypotension (20,22,50,54,56,59). Beck’s triad, which includes hypotension, elevated systemic venous pressure (jugular venous distention), and muffled heart sounds, are signs of cardiac tamponade. Additionally, a “bruit de Moulin” splashing murmur is suggestive of a hemopneumopericardium as the sound is caused by the movement of blood and air in the pericardium. Sudden hypotension or shock following a change in position may indicate a ruptured pericardium with herniation of the heart resulting in strangulation. This sudden onset coupled with the rarity of this presentation often results in cardiac herniation being missed until the patient becomes severely symptomatic or hemodynamically unstable. Other signs that indicate cardiac herniation include intermittent loss of pulse, maximum heart sounds in abnormal locations, and resolution of symptoms with a change of position (8,10,21,55,60,61).
Arrhythmias and commotio cordis
Several factors have been implicated in the development of arrhythmias including catecholamine release, acid-base changes, electrolyte imbalance, pre-existing anemia, hypovolemia, and substance use. Arrhythmias are common after cardiac contusion occurring in up to 70% of patients within 3 days of hospitalization for BCT. RBBB is thought to be the most common arrhythmia associated with cardiac contusion potentially due to the anterior location of the right side of the heart. Other described arrhythmias include sinus tachycardia, uniform premature ventricular complexes (PVC), multifocal PVC, atrial fibrillation (AF), LBBB, atrioventricular (AV) block, ventricular fibrillation (VF), ventricular tachycardia (VT), and supraventricular tachycardia (SVT) (3,8,18,20,24). Sinus tachycardia is the most common arrhythmia among trauma patients, having a role in compensating for volume loss and prevalence among patients experiencing pain. After sinus tachycardia, AF is the next most common arrhythmia. Paroxysmal supraventricular tachycardia (PSVT) is a rare but severe arrhythmia related to trauma that may result in heart failure, myocardial ischemia, or pulmonary edema if left untreated. While these patients may present with symptoms of trauma as previously described, symptoms of arrhythmias may include being asymptomatic, experiencing palpitations, chest pain, diaphoresis, shortness of breath, and syncope (1,2,9,20,24).
Dysrhythmias can be caused by BCT as previously described, but in the case of children, sports injuries are most prevalent. Blunt trauma to the chest with sports equipment such as hockey pucks, baseballs, and footballs have been described to cause arrhythmias. The most dangerous of these arrhythmias is commotio cordis which is sudden death caused by induction of VF. The impact is thought to occur during repolarization which is a vulnerable phase of electrical conduction and causes VF immediately after impact. In these cases, some patients were found not to have any other lethal injuries at the time of death. As commotio cordis may occur with relatively mild trauma and the sudden onset in nature, prediction of commotio cordis is nearly impossible. Additionally, if immediate first aid is not administered patients do not survive long enough to present to hospital for evaluation. Arrhythmias can also be caused by structural changes to the heart after injury. This group of injuries is called contusio cordis. Common rhythm abnormalities with contusio cordis include heart block and VF (1,5,24,62).
Evaluation and treatments of blunt cardiac trauma
Cardiac contusions
As there is often variability in severity and presentation of cardiac contusions, various diagnostic modalities have been utilized in order to aid the evaluation and treatment process. Cardiac contusions are characterized by injury to the myocardium. Cardiac enzymes such as creatinine kinase (CK) and troponin, enzymes that are released after an injury to the heart, have traditionally been used in evaluating patients for MI. They have also been utilized in the evaluation of cardiac trauma as both can be increased as a result of injury to the heart. CK is often released from skeletal muscle as well and so is less specific for cardiac damage, especially in the context of multi-system trauma as is often seen with BCT (3,8,18,21,30).
Electrocardiogram (ECG) provides information regarding the electrical function of the heart. Severe cardiac contusions are often associated with arrhythmias, therefore, ECG is an essential part of the diagnostic workup. A normal ECG can often help to rule out significant injuries (20).
Imaging has been utilized in order to identify structural damage to the heart after BCT. Echocardiography provides functional and structural assessments of the heart and is important for ruling out other injuries to the heart including valvular dysfunction, septal or free wall rupture, cardiac tamponade, and muscle function. Cardiac magnetic resonance imaging (MRI) is another option for the diagnosis of cardiac abnormalities with the ability to provide information regarding the extent of myocardial contusion and regional infarcts (2,3,53).
Diagnosis of cardiac contusions is often made on histopathologic samples. Mild trauma may present with grouped petechiae. Moderate injury may result in findings of ecchymoses of the epicardium. Severe trauma and ecchymosis often result in large areas of myocardial necrosis. Large or severe injuries may progress from necrosis to aneurysmal formation, pseudoaneurysms of a cardiac chamber, or direct rupture (10,20,51).
Management of cardiac contusions is often supportive therapy with the treatment of any underlying structural damage or new arrhythmias. Additional therapies that have been described include nitroglycerine and other vasodilators for the development of angina pectoris, anti-arrhythmic medications such as beta-blockers, and myocardial protection may be considered by restricting fluid and salt intake, as well as the administration of steroids and diuretics (8).
Valvular injuries
Findings of valvular injuries include widened mediastinum on chest X-ray (CXR) and increased troponin. Diagnosis of valvular injury often relies on transthoracic or transesophageal echocardiograms (1,9,17,19,28,35,39,63). Echocardiography is the fastest and most accurate modality for evaluating heart valves. While performing echocardiography in the context of trauma, care should be taken to examine the aorta and other surrounding structures that may have been injured with blunt trauma (26,29). Further evaluation for MR can be conducted using a Swan-Gantz catheter in order to measure left-sided heart pressures (39).
Early evaluation and surgical intervention are important for short and long-term outcomes. Surgical repair of injured cardiac valves has even demonstrated positive remodeling of the heart chambers (9,28,29,64,65). Aortic valve replacement (AVR) is an effective treatment for acute traumatic AR and has led to positive outcomes in patients who are stable and reach the operating room with mortality rates as low as 1% (17,29). The MV and TV often require replacement but may be repaired using annuloplasty rings and neochords, depending on the mechanism of injury (19,28,29,35,65).
Coronary injuries
Coronary angiography is the most effective way to diagnose coronary artery dissection, aneurysm, or rupture. Angiography is indicated when there is suspected injury to the coronary arteries or if there are signs of MI on ECG. CT angiography (CTA) is another imaging modality used to identify coronary injury (8,9,15,20). Doppler echocardiography can also be used to identify coronary rupture (64). Coronary injury may also be evaluated with laboratory tests such as the cardiac enzymes CK and troponin. Since troponin is elevated with other cardiac injuries such as cardiac contusion, and CK with skeletal muscle injuries, their specificity for identifying coronary injuries is limited (1-3,5,7,8,18,20,21). Additionally, coronary artery injury can result in arrhythmias and signs of infarct. ECG should be performed in all patients suspected of cardiac trauma and signs of MI or arrhythmias should raise the suspicion of coronary injury. Coronary vasospasm is thought to be one of the causes of commotio cordis, a lethal consequence of BCT (5,9,15,20,60).
Cardiac motion abnormalities isolated to an area supplied by a single coronary artery and hemopericardium or cardiac tamponade should increase the suspicion for coronary injury (20). Although, echocardiography can provide false negatives in this context if there is a pericardial injury and blood is draining into the thoracic cavity. A pericardial window may assist in the diagnosis in these cases. This is performed by creating an incision over the xiphoid process, dissecting into the retrosternal space, and opening the pericardium inspecting for blood. Patients with a positive finding with a pericardial window should receive a sternotomy for further investigation of the source of bleeding (41).
Treatment of coronary artery injury and its consequences vary by the injury type and presentation. Typically, patients with angina are initially treated with nitroglycerin or other vasodilators. Relief with the use of nitroglycerin can help to differentiate between myocardial ischemia and other causes of chest pain clinically. Arrhythmias can be controlled by medication such as beta-blockers or calcium channel blockers, although these should be used carefully in the context of traumatic injury to the heart (8). Coronary occlusion and dissection often need to be managed with percutaneous coronary intervention (PCI) or surgical revascularization through coronary artery bypass grafting (CABG) (1,2,5,7). One consideration prior to intervention for patients with coronary artery occlusion or dissection caused by trauma is the use of antiplatelet and anticoagulation therapy in coronary interventions. As patients who have experienced trauma may have multiple injuries, the introduction of anticoagulation may exacerbate any current bleeding or prevent the achievement of hemostasis. The benefits of intervention must be considered in the context of bleeding risks in these populations before attempting to repair the coronary arteries (20).
Aortic injuries
Evaluation of traumatic aortic injury begins with history and physical exam. Patients should be stabilized initially before conducting further examination. Signs of aortic injury on clinical evaluation include tachycardia, hypotension, chest or back pain, significant differences in limb blood pressure, and syncope (20,22,42). Initially, investigations in patients presenting with traumatic aortic injury should receive an ECG and cardiac enzymes should be monitored. On CXR, a widened mediastinum is a sign of aortic dissection. CXR is useful in this context as it is rapid and readily available, but it is not sufficient to make a definitive diagnosis (66). Echocardiography is a useful and relatively fast imaging modality for evaluating aortic injury. CT is the most commonly used method for diagnosing aortic dissection due to its combination of specificity and relative availability, although patients should be stabilized before sending for imaging. MRI is the most specific method for diagnosing aortic dissection but is limited in its utility in the setting of trauma due to relatively limited availability and length of imaging time (5,9,40,42,45).
There are three main options for treating an aortic injury. The first is pharmacotherapy with the goal of stabilization and prevention of progression of the aortic injury. This includes the use of beta-blockers in order to lower heart rate and blood pressure to prevent or slow further injury of the aorta. If the use of beta-blockers is contraindicated, calcium channel blockers can be used to the same effect. If monotherapy is not sufficient to reach target heart rate or blood pressure, nitroglycerin or nitroprusside can be used as an adjunct. Risks of treating aortic injuries with medical management include higher risk of disease progression (41).
The second approach is endovascular repair. This involves the placement of an endovascular stent inside of the aorta through a catheter-based approach allowing for repair with a minimally invasive approach. While endovascular repair is associated with lower short-term mortality and paraplegia than open repair, it was also associated with a slightly higher risk of stroke (5,8).
The third option is open surgical repair. The approach is most often a sternotomy and surgical repair or replacement of the damaged segment of the aorta. Open surgical repair is the gold standard treatment for ascending aortic injuries. Risks of treating aortic injuries with open surgical repair include higher rates of short-term mortality and paraplegia (5,42).
Septal defects and free wall ruptures
Investigation of septal defects or free wall ruptures may include several diagnostic modalities. Rapid detection and treatment are essential as delays in treatment often result in significant morbidity and high rates of mortality. Initially, ECG should be performed in order to assess for arrhythmias, MI, or other cardiac injuries. Cardiac enzymes may be used, and monitored regularly for the first 24–48 hours, to evaluate cardiac injury (2,3,30,48).
Imaging is often the most useful diagnostic test. CXR provides information such as identifying pulmonary edema, widened mediastinum, pneumothorax, hemothorax, and hemopericardium. Echocardiogram is regularly used and can identify ASD, VSD, and free wall ruptures. Echocardiogram is also effective at identifying pericardial effusions, hemopericardium, cardiac tamponade, and assessing their severity. CT is another method often used to evaluate the cardiac structure. Free wall rupture and septal defects are visible on CT, although CT may not be appropriate in acutely unstable patients such as many of those with free wall rupture and traumatic septal defects. A more invasive option is the pericardial window which can be utilized to directly visualize the pericardium and heart to evaluate for rupture or bleeding (3,7,23,30,38,41,47,48,50,52).
Medical management is limited in its ability to treat a cardiac rupture. In certain cases, the use of pharmacotherapy can help stabilize a patient pre or postoperatively. Inotropes and vasopressors may be used in order to maintain cardiac output in the context of significant shunts or hypovolemia. Certain defects can increase the risk for thrombosis and so antiplatelet or anticoagulation therapy may be beneficial, although the use of blood thinners should be implemented cautiously in the context of trauma and active or recent bleeding (23).
Traumatic septal defect and free wall rupture almost exclusively require urgent surgical repair, with the exception of small, hemodynamically insignificant septal defects. Small defects are sometimes amenable to primary closure with sutures. Large septal defects are most commonly repair using patch closure, such as with a bovine pericardial or Dacron patch. The most common surgical incision used in this context is the sternotomy, as this provides superior visualization and exposure when compared to a right or left thoracotomy (3,6,9,30,38,47,50,52,53,55,67).
Hemopericardium and pericardial injuries
Initial investigation of a patient with blunt trauma to the chest and suspected pericardial injury includes ECG, serial cardiac enzymes, CXR, echocardiography, and CT. A shift in the electrical axis on ECG may indicate cardiac herniation or subluxation. Additionally, tachycardia or dysrhythmias may be found with pericardial injury or tamponade (9,22,54,60). Imaging is often required to make a diagnosis of injury involving the pericardium. CXR may demonstrate a widened mediastinum, pneumo or hemothorax, mediastinal hematoma, or shifted cardiac shadow which may indicate a pleuropericardial rupture and herniation of the heart into the pleural space. While CXR is a valuable tool, it is not sufficient for the diagnosis of pericardial injuries. Echocardiography is suited for this type of injury as it is effectively able to identify defects in the pericardium as well as fluid within the pericardium creating an effusion or tamponade. Although, echocardiography can result in false negatives if the pericardium is ruptured and blood is flowing out of the pericardium into the pleural spaces. CT is another modality often used in evaluating the pericardium. CT is effective in identifying defects in the pericardium, pericardial effusions, tamponade, and hemothorax (1,4,12,15,22,41,47,50,54-57,59,60).
Treatment of blunt trauma involving the pericardium varies by injury type. Medical management can be used to control the symptoms associated with pericardial injury but is rarely definitive. Typical treatments include fluid resuscitation for hypovolemia, norepinephrine, epinephrine, vasopressors among other medications to maintain blood pressure and adequate perfusion, blood transfusions for massive blood loss (15,55).
Bleeding from the pericardium into the pleural cavity requires repair of the defect causing bleeding and chest tubes to drain the blood in the pleural space. Cardiac herniation or subluxation through a pleuropericardial rupture often requires urgent surgical repair to relieve strangulation, reposition the heart, and close the defect using either a primary repair with sutures or patch closure. Cardiac tamponade is treated with pericardiocentesis, thoracotomy, subxiphoid approach, or sternotomy to allow for pericardial drainage (6,8,9,15,41,42,52-57).
Arrhythmias and commotio cordis
Initially, evaluation of a trauma patient should include an ECG. ECG is the best method for diagnosing arrhythmia and may be used continuously in patients who have developed an arrhythmia or are at high risk. Some dysrhythmias experienced with cardiac trauma are dangerous and can result in rapid deterioration. Furthermore, structural damage to the heart is often associated in patients with severe blunt chest trauma and therefore further evaluation is necessary (2,20,24,68).
Some arrhythmias, such as sinus tachycardia, are part of a normal physiologic response and most often do not need to be treated. Sinus tachycardia can occur in the context of trauma due to increased pain or as a response to blood loss and hypovolemia. Treatment of sinus tachycardia should include treatment of underlying injuries such as volume resuscitation, pain management, and surgical repair of any injuries (20). Patients with rapid AF and hemodynamic instability should be cardioverted. For stable patients, pharmacotherapy with beta-blockers or calcium channel blockers may be effective and appropriate. These patients may also require anticoagulation prophylaxis to prevent clotting and embolization, but care should be taken to avoid starting anticoagulation in bleeding or at-risk patient. Patients experiencing PSVT should be treated urgently with vagal maneuvers, adenosine, beta-blockers, or cardioversion in order to address this arrhythmia. AV blocks are often transient in this patient population, but in cases where AV block is persistent, permanent pacemaker implantation may be necessary. Conduction abnormalities such as bundle branch blocks or complete atrioventricular node blocks are either transient or result in no long-term deleterious effects and often do not need to be treated. In persistent heart block, a pacemaker may be required (1,2,20,69,70). Commotio cordis is often not associated with structural injuries and so the focus has been placed on prevention. Improvement of chest protection during sporting activities has been pursued in an attempt to reduce this condition, although one study found that approximately 38% of patients who experienced commotio cordis were already wearing chest protection. Survival of commotio cordis is rare as treatment is most often administered on the scene by bystanders. Immediate treatment involves prompt and high-quality CPR and defibrillation with an automated external defibrillator (AED). Survival rates have improved with the improved CPR training of the general population and increased prevalence of AEDs (20,62,69-71).
Discussion
BCT is an uncommon and often underdiagnosed result of blunt trauma. Even so, BCT is thought to be responsible for approximately 25% of traumatic deaths. Several factors may contribute to high mortality rates and underdiagnosis. First, cardiac trauma often presents in cases of severe blunt trauma and is in the context of other distracting injuries. With the increasing severity of injuries comes an increased risk of morbidity and mortality. Second, cardiac injuries do not always present with symptoms initially, and even when symptoms are present, they are often not specific to a certain condition. Third, as highlighted by this review, numerous types of cardiac injury may occur in the context of blunt trauma that may occur individually or in various combinations (2,8-10,12-14).
These factors, coupled with high mortality rates before presentation to hospital, have created a field that is difficult to study. In contrast to naturally occurring diseases, such as isolated valvular disease, traumatic cardiac injury is complex and variable. Often isolated valve diseases occur with a set of common comorbidities, develops with a well understood pathophysiology, and are treated in large numbers in each center that allow for high-quality retrospective, prospective, and randomized control trial studies. In contrast, BCT has various presentations, injuries vary depending on the mechanism of injury and the patient, often multiple injuries involving the cardiac and other bodily systems, presentations to individual centers are sporadic and in small numbers, many patients do not present to care, and those that do have high rates of mortality. These factors make BCT difficult to study. This is reflected in the literature. The vast majority of publications regarding BCT are limited to individual case reports or case series with few retrospective studies. Without large studies on the evaluations, treatments, and outcomes of patients experiencing blunt cardiac trauma, producing effective guidelines is difficult.
Further study into blunt cardiac trauma is indeed warranted. While it may be difficult to produce retrospective or prospective studies at individual centers, there may be approaches that will allow the collection of this data. Extensive recording of data from BCT patients including their presentations, treatment, and outcomes will be helpful to continue building the collective knowledge regarding these injuries. The widespread establishment of multicenter or national databases, such as The National Commotio Cordis Registry, will allow for the opportunity to produce retrospective studies evaluating outcomes of BCT patients. Additionally, the use of guideline recommendations and frequent updates, coupled with large-scale data collection, will allow for continuous reevaluation of approaches to each of the injuries reviewed and updated recommendations that build on previous knowledge. These, among other approaches, should be undertaken to address the limitations in the field of BCT treatment and to continue to improve the outcomes of patients who experience these injuries.
Limitations
The most significant limitation of this review is the type of articles included. The vast majority of the literature published regarding BCT is in the form of case reports or series. Few retrospective and prospective studies with large numbers of patients have been published on this topic. This is likely due to the wide variation in patient presentation and that case rates at individual centers are sporadic and small in numbers. The establishment of national or multinational registries may aid in providing higher quality data and research into this topic moving forward. Additionally, risk of bias cannot be completely eliminated from any manuscript and the use of a single database may have contributed to the risk of bias if any manuscripts were published in other databases and not included in this review.
Conclusion
BCT is both rare and often missed. A wide variety of cardiac injuries are possible with blunt trauma ranging from rhythm abnormalities to structural damage such as cardiac contusions, septal or free wall rupture, and coronary dissection, to extra cardiac injuries such as aortic dissection or pericardial injury. Furthermore, literature regarding BCT is largely limited to case reports and few retrospective studies. Further study into BCT is necessary including the extensive recording of data from BCT patients including their presentations, treatment, and outcomes, the widespread establishment of multicenter or national databases, and the use of this data to produce large datasets and retrospective or prospective studies. The collection of this data may be used to identify optimal treatments for BCT patients. This data would address the limitations in the field of BCT treatment and continue to improve the outcomes of patients who experience these injuries.
Acknowledgments
We would like to thank Dawne Colwell, medical graphics designer, for the creation of the included figures.
Funding: University Hospital Foundation, University of Alberta.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Simon R. Turner) for the series “Traumatic Injuries of the Mediastinum” published in Mediastinum. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review Reporting Checklist. Available at https://dx.doi.org/10.21037/med-21-19
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/med-21-19). The series “Traumatic Injuries of the Mediastinum” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Leite L, Gonçalves L, Nuno Vieira D. Cardiac injuries caused by trauma: Review and case reports. J Forensic Leg Med 2017;52:30-4. [Crossref] [PubMed]
- Yousef R, Carr JA. Blunt cardiac trauma: a review of the current knowledge and management. Ann Thorac Surg 2014;98:1134-40. [Crossref] [PubMed]
- Karpas A, Yen K, Sell LL, et al. Severe blunt cardiac injury in an infant: a case of child abuse. J Trauma 2002;52:759-64. [Crossref] [PubMed]
- Gosavi S, Tyroch AH, Mukherjee D. Cardiac Trauma. Angiology 2016;67:896-901. [Crossref] [PubMed]
- Eghbalzadeh K, Sabashnikov A, Zeriouh M, et al. Blunt chest trauma: a clinical chameleon. Heart 2018;104:719-24. [Crossref] [PubMed]
- Baldwin D, Chow KL, Mashbari H, et al. Case reports of atrial and pericardial rupture from blunt cardiac trauma. J Cardiothorac Surg 2018;13:71. [Crossref] [PubMed]
- Hanschen M, Kanz KG, Kirchhoff C, et al. Blunt Cardiac Injury in the Severely Injured - A Retrospective Multicentre Study. PLoS One 2015;10:e0131362 [Crossref] [PubMed]
- Gao JM, Li H, Wei GB, et al. Blunt Cardiac Injury: A Single-Center 15-Year Experience. Am Surg 2020;86:354-61. [Crossref] [PubMed]
- Co SJ, Yong-Hing CJ, Galea-Soler S, et al. Role of imaging in penetrating and blunt traumatic injury to the heart. Radiographics 2011;31:E101-15. [Crossref] [PubMed]
- RuDusky BM. Classification of myocardial contusion and blunt cardiac trauma. Angiology 2007;58:610-3. [Crossref] [PubMed]
- Mullinix AJ, Foley WD. Multidetector computed tomography and blunt thoracoabdominal trauma. J Comput Assist Tomogr 2004;28:S20-7. [Crossref] [PubMed]
- Palas J, Matos AP, Mascarenhas V, et al. Multidetector computer tomography: evaluation of blunt chest trauma in adults. Radiol Res Pract 2014;2014:864369 [Crossref] [PubMed]
- Miller LA. Chest wall, lung, and pleural space trauma. Radiol Clin North Am 2006;44:213-24, viii. [Crossref] [PubMed]
- Verma N, White CS, Mohammed TL. Blunt Cardiothoracic Trauma: Common Injuries and Diagnosis. Semin Roentgenol 2018;53:171-7. [Crossref] [PubMed]
- Sabashnikov A, Michels G, Fatullayev J, et al. Coronary or ventricular rupture after blunt chest trauma? A clinical dilemma. Perfusion 2017;32:419-21. [Crossref] [PubMed]
- Oikonomou A, Prassopoulos P. CT imaging of blunt chest trauma. Insights Imaging 2011;2:281-95. [Crossref] [PubMed]
- Tsugu T, Murata M, Mahara K, et al. Long-Term Survival on Medical Therapy Alone after Blunt-Trauma Aortic Regurgitation: Report of a New Case with Summary of 95 Others. Tex Heart Inst J 2016;43:446-52. [Crossref] [PubMed]
- Huguet M, Tobon-Gomez C, Bijnens BH, et al. Cardiac injuries in blunt chest trauma. J Cardiovasc Magn Reson 2009;11:35. [Crossref] [PubMed]
- Pasquier M, Sierro C, Yersin B, et al. Traumatic mitral valve injury after blunt chest trauma: a case report and review of the literature. J Trauma 2010;68:243-6. [Crossref] [PubMed]
- Bock JS, Benitez RM. Blunt cardiac injury. Cardiol Clin 2012;30:545-55. [Crossref] [PubMed]
- Quintard H, Badia E, Duponq R, et al. Left cardiac luxation caused by a blunt chest trauma: a difficult diagnosis confirmed on chest computed tomography scan-two case reports. J Trauma 2010;68:E74-6. [Crossref] [PubMed]
- Chai HS, Lee SW, Park JS. Cardiac arrest associated with aortic valve regurgitation. Am J Emerg Med 2018;36:345.e1-e3. [Crossref] [PubMed]
- Behrle N, Dyke P, Dalabih A. Interventricular Septal Pseudoaneurysm After Blunt Chest Trauma in a 6 Year Old: An Illustrative Case and Review. Pediatr Emerg Care 2018;34:e39-40. [Crossref] [PubMed]
- Sakka SG, Huettemann E, Giebe W, et al. Late cardiac arrhythmias after blunt chest trauma. Intensive Care Med 2000;26:792-5. [Crossref] [PubMed]
- Hashmi ZA, Maher TD, Sugumaran RK, et al. Acute aortic valve rupture secondary to blunt chest trauma. J Card Surg 2010;25:381-2. [Crossref] [PubMed]
- Hill GED, Thorsen TN, Goelz AP, et al. A Rare Consequence of Remote Blunt Chest Trauma. J Cardiothorac Vasc Anesth 2019;33:2875-81. [Crossref] [PubMed]
- Stahl RD, Liu JC, Walsh JF. Blunt cardiac trauma: Atrioventricular valve disruption and ventricular septal defect 1466 CASE REPORT. Ann Thorac Surg 1993;105:1466-8.
- Parsaee M, Saedi S, Porkia R. Peri-mitral ventriculoatrial fistula after blunt thoracic trauma. Echocardiography 2018;35:895-7. [Crossref] [PubMed]
- Prêtre R, Faidutti B. Surgical management of aortic valve injury after nonpenetrating trauma. Ann Thorac Surg 1993;56:1426-31. [Crossref] [PubMed]
- Sabzi F, Niazi M, Zokaei AH, et al. Ventricular septal necrosis after blunt chest trauma. J Inj Violence Res 2012;4:98-100. [Crossref] [PubMed]
- Lamela Domenech AE, Lopez-Menendez F, López-Candales A. Tricuspid Papillary Muscle Rupture Due to Blunt Chest Trauma. J Ultrasound Med 2016;35:2733-6. [Crossref] [PubMed]
- Stoica B, Paun S, Tanase I, et al. Traumatic Tricuspid Valve Rupture after Blunt Chest Trauma - A Case Report and Review of the Literature. Chirurgia (Bucur) 2015;110:467-70. [PubMed]
- Ismailov RM, Weiss HB, Ness RB, et al. Blunt cardiac injury associated with cardiac valve insufficiency: trauma links to chronic disease? Injury 2005;36:1022-8. [Crossref] [PubMed]
- Branch CF, Adams J. Left ventricular rupture with resulting cardiac tamponade due to blast force trauma from gunshot wound. J Emerg Med 2012;43:263-5. [Crossref] [PubMed]
- Saric P, Ravaee BD, Patel TR, et al. Acute severe mitral regurgitation after blunt chest trauma. Echocardiography 2018;35:272-4. [Crossref] [PubMed]
- Lambrechts DL, Wellens F, Vercoutere RA, et al. Early stabilization of traumatic aortic transection and mitral valve regurgitation with extracorporeal membrane oxygenation. Tex Heart Inst J 2003;30:65-7. [PubMed]
- Misfeld M, Ehlermann P, Sievers HH. Transaortic repair of blunt traumatic cardiac wall and papillary muscle rupture. J Thorac Cardiovasc Surg 2001;122:834-5. [Crossref] [PubMed]
- Wu JJ, Yu TJ, Wang JJ, et al. Early repair of traumatic ventricular septal defect and mitral valve regurgitation. J Trauma 1995;39:1191-3. [Crossref] [PubMed]
- Varahan SL, Farah GM, Caldeira CC, et al. The double jeopardy of blunt chest trauma: a case report and review. Echocardiography 2006;23:235-9. [Crossref] [PubMed]
- Yang S, Wang C, Chen H. Partial aortic annulus avulsion and formation of aortic-left ventricle tunnel through interventricular septum after blunt cardiac trauma. Eur J Cardiothorac Surg 2011;40:255-6. [Crossref] [PubMed]
- Gough JD, Yee MK. Mediastinal trauma--or not? Anaesthesia 1989;44:869. [Crossref] [PubMed]
- Sun X, Hong J, Lowery R, et al. Ascending aortic injuries following blunt trauma. J Card Surg 2013;28:749-55. [Crossref] [PubMed]
- Kutsukata N, Sakamoto Y, Mashiko K, et al. Morphological evaluation of areas of damage in blunt cardiac injury and investigation of traffic accident research. Gen Thorac Cardiovasc Surg 2012;60:31-5. [Crossref] [PubMed]
- Shenoy KS, Jeevannavar SS, Baindoor P, et al. Fatal blunt cardiac injury: are there any subtle indicators? BMJ Case Rep 2014;2014:bcr2013203149 [Crossref] [PubMed]
- Sammer M, Wang E, Blackmore CC, et al. Indeterminate CT angiography in blunt thoracic trauma: is CT angiography enough? AJR Am J Roentgenol 2007;189:603-8. [Crossref] [PubMed]
- Kanchan T, Menezes RG, Sirohi P. Penetrating cardiac injuries in blunt chest wall trauma. J Forensic Leg Med 2012;19:350-1. [Crossref] [PubMed]
- Ch'ng S, Plunkett B, Hardikar A, et al. Blunt cardiac rupture in the setting of previous sternotomy. Ann Thorac Surg 2012;94:1343-5. [Crossref] [PubMed]
- Nakajima H, Uwabe K, Asakura T, et al. Emergent surgical repair of left ventricular rupture after blunt chest trauma. Ann Thorac Surg 2014;98:e35-6. [Crossref] [PubMed]
- Maraqa T, Mohamed MAT, Wilson KL, et al. Isolated right atrial rupture from blunt trauma: a case report with systematic review of a lethal injury. J Cardiothorac Surg 2019;14:28. [Crossref] [PubMed]
- Ryu DW, Lee SY, Lee MK. Rupture of the left atrial roof due to blunt trauma. Interact Cardiovasc Thorac Surg 2013;17:912-3. [Crossref] [PubMed]
- Pollak S, Stellwag-Carion C. Delayed cardiac rupture due to blunt chest trauma. Am J Forensic Med Pathol 1991;12:153-6. [Crossref] [PubMed]
- Ball CG, Peddle S, Way J, et al. Blunt cardiac rupture: isolated and asymptomatic. J Trauma 2005;58:1075-7. [Crossref] [PubMed]
- Al Ayyan M, Aziz T, El Sherif A, et al. Blunt cardiac injury: case report of salvaged traumatic right atrial rupture. Ulus Travma Acil Cerrahi Derg 2015;21:527-30. [PubMed]
- Kamiyoshihara M, Nagashima T, Ibe T, et al. Rupture of the diaphragm and pericardium with cardiac herniation after blunt chest trauma. Gen Thorac Cardiovasc Surg 2010;58:291-4. [Crossref] [PubMed]
- Nhan NH, Anh PT, Trung TM, et al. Blunt traumatic left atrial appendage rupture and cardiac herniation. Asian Cardiovasc Thorac Ann 2014;22:598-600. [Crossref] [PubMed]
- Rodgers-Fischl PM, Makdisi G, Keshavamurthy S. Extrapericardial Tamponade After Blunt Trauma. Ann Thorac Surg 2021;111:e49-50. [Crossref] [PubMed]
- Sohn JH, Song JW, Seo JB, et al. Case report: pericardial rupture and cardiac herniation after blunt trauma: a case diagnosed using cardiac MRI. Br J Radiol 2005;78:447-9. [Crossref] [PubMed]
- Janson JT, Harris DG, Pretorius J, et al. Pericardial rupture and cardiac herniation after blunt chest trauma. Ann Thorac Surg 2003;75:581-2. [Crossref] [PubMed]
- Dokoupil M, Marecová K, Uvíra M, et al. Fatal delayed hemopericardium and hemothorax following blunt chest trauma. Forensic Sci Med Pathol 2019;15:272-5. [Crossref] [PubMed]
- Sherren PB, Galloway R, Healy M. Blunt traumatic pericardial rupture and cardiac herniation with a penetrating twist: two case reports. Scand J Trauma Resusc Emerg Med 2009;17:64. [Crossref] [PubMed]
- Wall MJ Jr, Mattox KL, Wolf DA. The cardiac pendulum: blunt rupture of the pericardium with strangulation of the heart. J Trauma 2005;59:136-41; discussion 141-2. [Crossref] [PubMed]
- Marshall DT, Gilbert JD, Byard RW. The spectrum of findings in cases of sudden death due to blunt cardiac trauma--'commotio cordis'. Am J Forensic Med Pathol 2008;29:1-4. [Crossref] [PubMed]
- Mehrotra D, Dalley P, Mahon B. Tricuspid valve avulsion after blunt chest trauma. Tex Heart Inst J 2012;39:668-70. [PubMed]
- Türk EE, Tsokos M. Blunt cardiac trauma caused by fatal falls from height: an autopsy-based assessment of the injury pattern. J Trauma 2004;57:301-4. [Crossref] [PubMed]
- Cheng Y, Yao L, Wu S. Traumatic Tricuspid Regurgitation. Int Heart J 2017;58:451-3. [Crossref] [PubMed]
- Vasileiou G, Qian S, Al-Ghamdi H, et al. Blunt Trauma: What Is Behind the Widened Mediastinum on Chest X-Ray (CXR)? J Surg Res 2019;243:23-6. [Crossref] [PubMed]
- Miner J, Kirkland J, Hardman C, et al. Blunt rupture of two cardiac chambers following a motor vehicle collision. J Trauma Acute Care Surg 2019;87:736. [Crossref] [PubMed]
- Cureton EL, Yeung LY, Kwan RO, et al. The heart of the matter: utility of ultrasound of cardiac activity during traumatic arrest. J Trauma Acute Care Surg 2012;73:102-10. [Crossref] [PubMed]
- Capucci A, Aschieri D, Piepoli MF, et al. Tripling survival from sudden cardiac arrest via early defibrillation without traditional education in cardiopulmonary resuscitation. Circulation 2002;106:1065-70. [Crossref] [PubMed]
- Myerburg RJ, Velez M, Rosenberg DG, et al. Automatic external defibrillators for prevention of out-of-hospital sudden death: effectiveness of the automatic external defibrillator. J Cardiovasc Electrophysiol 2003;14:S108-16. [Crossref] [PubMed]
- Doerer JJ, Haas TS, Estes NA 3rd, et al. Evaluation of chest barriers for protection against sudden death due to commotio cordis. Am J Cardiol 2007;99:857-9. [Crossref] [PubMed]
Cite this article as: EL-Andari R, O'Brien D, Bozso SJ, Nagendran J. Blunt cardiac trauma: a narrative review. Mediastinum 2021;5:28.


