Transmediastinal penetrating trauma
Introduction
Penetrating injuries traversing the mediastinum pose an extremely challenging situation for those caring for injured patients. Owing to the critical structures within this region, these injuries carry a very high mortality rate (1). These injuries are most frequently caused by firearms, although they may also be caused by missiles from other sources or impalements (2-4). While many patients die at the scene, the advent of better trauma systems and rapid pre-hospital transport times has resulted in many arriving to hospital with high-risk, but potentially salvageable, injuries (1).Other patients, it is now well recognized, will arrive to hospital with transmediastinal penetrating trauma but without a life-threatening injury (2,3). Thus, a high degree of efficiency is needed to rapidly assess and identify those patients requiring operative intervention. Patients with transmediastinal injuries (TMIs) once mandated surgical exploration or a complex, invasive set of investigations, but this has evolved with the development of high-resolution computed tomography (CT) scanning and series from high volume trauma centers showing the safety of a tiered approach (2-4).
A TMI is defined as any traumatic injury that traverses or partially traverses the mediastinum (2). Common trajectories include transverse, anteroposterior, descending from the root of the neck, or oblique combinations of these (2). It is often difficult to be certain of the trajectory in the early stages of assessment. Clinical findings that may be indicative of a penetrating TMI include (3,5):
- Ballistic trauma with an entry wound and exit wound on opposite sides of the thorax;
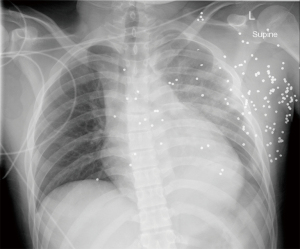
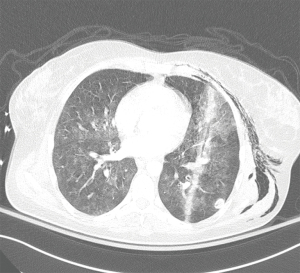
- Ballistic trauma with a single wound and imaging demonstrating a retained projectile on the contralateral side or within the mediastinum (Figure 1);
- A penetrating wound in the central thorax (2);
- Entry wound on one side of the thorax with hard signs of injury to mediastinal structures or the contralateral hemithorax (positive pericardial fluid on ultrasound or presence of blood in the contralateral chest tube).
While these are clinical findings suggestive of TMI during initial assessment, the degree of underlying injury is highly variable depending on the specific trajectory, making this determination a critical part of successful management of these patients. This article reviews the modern epidemiology, work up, and management of this injury pattern.
Methodology
A search of the PubMed database was conducted in December of 2020, encompassing peer-reviewed literature dating from 1966 to present day. General search criteria included the terms, “penetrating transmediastinal trauma”, “penetrating trauma to the chest”, “transmediastinal gunshot wounds”, and variants of these terminology. The purpose of this chapter is to provide a literature review on the topic of penetrating transmediastinal trauma with informed appraisal of the literature by expert opinion. The majority of the literature on this topic is derived from high volume tertiary care trauma centers in the United States.
Epidemiology
Transmediastinal penetrating trauma is a relatively rare injury pattern and can result from firearms, stabbings, other missiles, and blast injuries (1,3,5,6). The most predominant source, however, remains firearms, accounting for the vast majority of these injuries (3). A retrospective analysis of patients admitted with penetrating mediastinal trauma between 1997 and 2003 at a level one trauma center demonstrated a mortality rate of 42% for patients with gunshot wounds and 7% for those with stab wounds (7).In one large series from Los Angeles, where transport times are very short, the overall mortality of patients with confirmed transmediastinal gunshot injuries was 78.9%. Of those who reached the hospital with vital signs, mortality was 24.3% (1). The majority of patients with TMI are male (80–94%), which reflects the general population of patients with firearms-related injury (1,3). The incidence of TMIs is thought to parallel the availability of firearms and firearm-related violence (8). Although rare, patients presenting with multiple transmediastinal gunshot wounds present an even greater diagnostic challenge in determining trajectories and have a very poor prognosis.
The underlying injury pattern that has been reported varies, likely as a result of the center’s typical transport time which can create a survivorship bias towards certain injuries. Cardiac injuries are consistently the most commonly reported (1,3,7,8). In one large American retrospective study conducted from 2006–2010, of 133 patients with a transmediastinal gunshot wound, 70% had a cardiac injury (1). The next most common injuries were to the thoracic aorta (24.1%) and pulmonary (21.8%). The esophagus and trachea are often spared, with tracheobronchial injuries being exceptionally rare (1,8).
With the increasing availability of firearms in the late 20th century, the incidence of penetrating thoracic trauma markedly increased and then stabilized over time (7). Firearm injuries and stabbings account for more than half of penetrating thoracic injuries in the United States (7,9,10). The number of people who die from transmediastinal penetrating trauma is unknown (11). Large autopsy studies of individuals who died of trauma before reaching hospital suggest penetrating chest trauma is a major cause of prehospital death. One such study from Miami-Dade County in the United States showed that of 512 deaths over a one-year period, 42.8% were from firearms. Of this population, the most commonly injured body area was the brain followed closely by the chest (54.1%). 25% of patients had cardiac injuries, and 21% had injury to major thoracic vascular injuries, implying that many patients with TMIs never make it to hospital (12).
Historical perspective
Early case series on the management of battlefield casualties supported the notion of mandatory surgical exploration in patients sustaining penetrating abdominal or thoracic gunshot wounds (4,6). In the United States, this approach was utilized at major trauma centers during the increasing incidence of non-military-grade handgun violence in the 1970s (7,13). However, the difference between military and civilian weaponry, availability of diagnostic resources, logistics, and financial burden, brought into question the utility and harms of this approach. Furthermore, intraoperative findings demonstrated a high false negative rate (1,4,5). While it remained generally agreed upon that patients with florid hemodynamic instability warranted immediate surgical exploration, many authors proposed a triaged approach to decrease the number interventions which were time-consuming, expensive, invasive, and often unnecessary (3,5).
The biggest changes in the care of patients with TMI injury pattern have been with regards to the diagnostic workup and management of stable patients. While even in these patients, mandatory surgical exploration or invasive tests used to be the rule, the current paradigm takes advantage of improved tomographic imaging to guide management (1,3,6). This has partly been driven by modern CT imaging, which can accurately offer information on missile trajectory and screen for injury to all mediastinal organs (2,5). Before the 21st century, the standard diagnostic workup for hemodynamically stable patients on initial evaluation often included chest radiography, angiography, esophagography, bronchoscopy, esophagoscopy, and pericardial window (5,7). There was controversy regarding the diagnostic sequence of investigations, which were often time-consuming, with some centers advocating for aortic angiography before esophagography, while others center supported the contrary (3,8). Proponents of an esophagus-first strategy believed that most patients with aortic injuries were symptomatic—usually with hemodynamic compromise—and thus argued that the yield of angiography in these patients was low and not worth delaying diagnosis of an esophageal injury (14).
At the end of the 20th century, several large series showed that CT imaging in hemodynamically stable patients was effective in identifying missile trajectory, which could then be used to guide subsequent investigations and management (5,15). If the missile trajectory was found to be sufficiently close to a mediastinal organ this would warrant additional, more specific investigation or intervention (16). This CT-guided approach to diagnostic workup was shown to decrease the number of investigations, be beneficial from a cost perspective, and was not associated with higher rates of missed injuries (17). Finally, the technological improvements in bedside ultrasound and increasing provider experience with this modality have allowed for rapid and accurate assessment of the pericardium, decreasing the need for pericardial windows in the hemodynamically stable patient (18).
Management
The initial approach to patients with penetrating thoracic trauma begins with a rapid primary survey as organized and advocated by the Advanced Trauma Life Support (ATLS) curriculum (19). Many patients with TMI will present in extremis. In one large study from a US trauma center, patients were stratified by first measured systolic blood pressure (SBP): >100, 60–100, and <60 mmHg. Half of patients with transmediastinal penetrating trauma presented with an SBP <60 and were immediately explored surgically. The remaining two groups accounted for 20% and 30% of cases respectively (3). Similarly, another series of transmediastinal gunshots classified 87% of 133 patients as unstable or dead on arrival (1). Thus, the rapid, systematic approach advocated by ATLS is essential given the majority of patients presenting with profound hemodynamic instability (1,3). The authors agree with the triage of patients based on systolic blood pressure measurements, and in practice, this provides a simple and effective measure to determine prompt hemodynamic instability and subsequent management.
With penetrating injuries, it is imperative to search for the location of all external wounds early in the assessment as this will determine which areas of the body might be injured and help inform trajectory. Chest X-ray (CXR) and extended focused assessment with sonography in trauma (eFAST) are adjunctive tools that should be performed early since they can rapidly identify the presence of intraabdominal and intrathoracic findings. CXR findings in combination with clinical features are useful in determining the suspected trajectory of penetrating injuries in the thoracic cavity. Any embedded foreign bodies should be left in situ and carefully bolstered to avoid being dislodged or transmitting force to internal structures (19).
Chest tube thoracostomy should be used liberally in the setting of penetrating thoracic trauma, especially if TMI is suspected. This procedure is both therapeutic and diagnostic, treating hemothorax and pneumothorax while also providing information through the chest tube output. Some sources have suggested that the quantity of chest tube output may be an indication for operative management, but this absolute volume is less important than the hemodynamic status of the patient and knowledge of the underlying injuries (7,19).
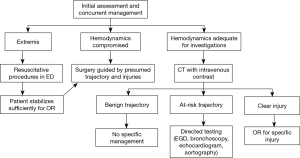
Once initial assessment is performed, the patient is classified into a tiered system based on their physiologic stability. Although the definition of “hemodynamically stable” is variable, it is usually based on a combination of blood pressure and heart rate, but may also consider chest tube output, presence of tamponade, or visible blood loss (1,3,5,20). Patients can generally be categorized into those in extremis, those who are hemodynamically compromised or unstable, and those who are sufficiently stable to undergo further investigations. This helps guide further management. Many authors have proposed similar algorithms based on hemodynamics and one such approach is summarized in Figure 2 (20-22).
Patients in extremis
Patients who have lost vital signs or who are peri-arrest are generally treated with a resuscitative thoracotomy or clamshell thoracotomy (23,24). These exposures allow for several potentially life-saving maneuvers including decompressing cardiac tamponade, repairing cardiac injuries, cross-clamping the thoracic aorta, and controlling vascular injuries. Although mortality remains high, survival rates of 2.8–14.3% have been reported for TMIs specifically (1,7,8).
Patients with hemodynamic compromise
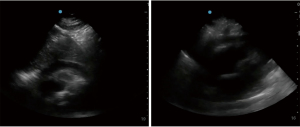
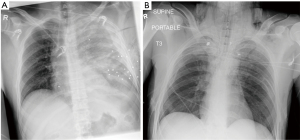
Patients with unstable vital signs or who fail to respond to initial attempts at resuscitation require immediate operative management (25). Similarly, those found to have hard signs of injury such as pericardial fluid on eFAST (Figure 3)or high amounts of bloody output from their chest tubes require emergent operative management. Priority must be placed on rapidly getting the patient to definitive hemorrhage control, a task best achieved in the operating room (25). Imaging will be limited to supine X-rays and eFAST exam, both available in the trauma bay. These investigations are extremely important, even in the unstable patient, because they can help establish missile trajectory and assess specific body cavities for evidence of bleeding (Figure 4A,B). This, in turn, helps the surgeon make an educated decision on how to sequence the operation and what structures may be at risk (1).
While moving towards definitive hemorrhage control, permissive hypotension and hemostatic resuscitation are important resuscitative paradigms. In permissive hypotension, instead of aggressively infusing fluids and blood to correct low blood pressure, the team tolerates hypotension and uses blood products judiciously until definitive hemorrhage control is in reach. In one landmark trial, 598 patients with SBP ≤90 and penetrating torso injury were randomized to either standard fluid resuscitation or a fluid-minimizing arm (26). Mortality was significantly lower in the group that received minimal fluid or blood products before reaching the operating room (26). Increasing blood pressure before injuries have been controlled may exacerbate the injury by disrupting an unstable clot or by increasing the rate of blood loss. In hemostatic resuscitation, crystalloid and colloid is avoided in favor of blood products. While the patient is unstable, these products are administered in a fixed ratio approaching whole blood. If available, viscoelastic hemostatic assays and conventional coagulation tests may be used to help guide resuscitation. The widespread use of massive hemorrhage protocols facilitates adherence to this principle (27,28).
Careful judgement must be exercised with regards to which incision will optimize control and repair of injuries. The surgeon must use knowledge about the hypothesized trajectory, results of limited imaging, chest tube output, and anticipation of resuscitative maneuvers such as aortic cross-clamping to select the best approach. Because of the inherent uncertainty surrounding the underlying injuries and the likelihood that injuries exist in both hemithoraces, the patient should initially be positioned supine with arms abducted to 90 degrees. A choice is then made between left or right anterolateral thoracotomy, bilateral anterolateral (clamshell) thoracotomy, and median sternotomy, considering their ability to expose structures and their extensibility.
Review of specific procedures and repair of specific injuries are beyond the scope of this review.
Patients with hemodynamics adequate for investigations
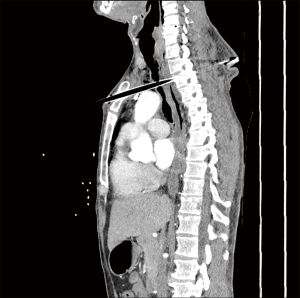
Stable patients should be cautiously and expeditiously investigated to determine underlying injuries. At our institution, a CT angiogram (CTA) of the chest is the initial imaging modality of choice, allowing for identification of missile trajectory through the mediastinum and identification of some injuries to underlying structures (Figures 5-7). CTA serves as an effective screening tool, with positive findings guiding further management or diagnostic work-up. Studies have demonstrated that in the absence of mediastinal injury or threatening trajectory on CT, the patient can be safely managed non-operatively and without further investigations of mediastinal organs (2,4). With missiles, trajectories are generally linear, but projectiles may fragment within the body or alter course when they deflect on bone or fascia (29). These may contribute to difficulty in evaluation of trajectory (4). Projectile embolization is another rare phenomenon observed in which the projectile breaches a vascular structure and travels to a distant location from its entry point (29).
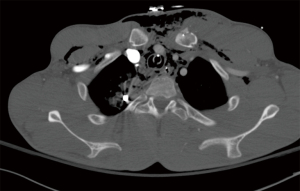
Vascular injuries from transmediastinal penetrating trauma carry a high mortality rate, with the ascending aorta, aortic arch, and great vessels as common injury sites (2,30). In the stable trauma patient, CTA is an effective and highly accurate diagnostic tool, replacing the use of catheter-based aortography and transesophageal echocardiography (TEE) (31-33). In the patient stable enough to undergo CTA, the study may show pseudoaneurysm, vascular occlusion, intimal flap, or active extravasation (2,4,30). Rapid identification of such findings enables operative or angiographic planning and prompt therapeutic intervention. Most large trauma centers now use CTA as the imaging modality of choice for diagnosing thoracic vascular injuries since it is rapid, non-invasive, and provides information on other structures (34). Angiography is reserved for situations where more detail is needed or if artefact from metallic fragments creates too much distortion for CTA to be informative (34).
While most cardiac injuries following TMI are devastating and lead to rapid exsanguination or tamponade (1), injuries may still be present in the stable patient (12,24,35). CXR may demonstrate an enlarged cardiac contour, presence of hemothorax, or widened mediastinum but these findings are neither sensitive nor specific (36,37). eFAST is an excellent tool to evaluate for pericardial fluid with strong test characteristics (38-40). The known major exception to its sensitivity for significant cardiac injury is in the setting of an injury that is decompressing into the pleural cavity (41). Thus, for patients with a suspected cardiac injury and a left hemothorax, it is advocated that these patients still undergo a more definitive test such as subxiphoid pericardial window (40). Chest CT has demonstrated high accuracy for detection of cardiac injury by accurately assessing for hemopericardium, pneumopericardium, contrast extravasation, or presence of intracardiac foreign body, with the higher number of positive findings correlating with increasing sensitivity and specificity of the test (42-46). In the presence of both myocardial and pericardial defects, there is no pericardial accumulation of fluid, thus relying on the presence of pericardial effusion alone to detect cardiac injury is insufficient (41). Finally, pericardial window, either subxiphoid or transdiaphragmatic, remains a reliable and extremely accurate diagnostic test for cardiac injury (43). It is particularly useful in patients where subcutaneous emphysema makes ultrasonography of the heart impossible or a cardiac injury may be draining into the pleural space (26,43).
Esophageal injury presents a diagnostic challenge and can often be present despite initial hemodynamic stability, with delayed detection associated with increased mortality (47,48). On CT, the identification of a projectile or projectile trajectory within close proximity of the esophagus should warrant clinical suspicion. Although the presentation is often innocuous and clinical features are unreliable within the context of trauma, dysphagia, hematemesis, or stridor may be present (47,48-55). A dreaded complication of such injury is mediastinitis, carrying a high mortality. On CXR, classic findings include a left-sided pleural effusion and soft tissue emphysema but these findings are neither sensitive nor specific (48). Initial CTA findings such as air bubbles around the esophagus, thickening of the esophageal wall with adjacent inflammatory stranding, and discontinuity of the wall carry are suggestive of injury (14,49-53). Where uncertainty exists, injury is best assessed with either esophagoscopy or esophagography. When trained endoscopists are available, modern data has shown that flexible esophagoscopy has favourable test characteristics with sensitivity and specificity for traumatic injury consistently over 95% (48,49). Endoscopy is widely available and, when necessary, can be performed at the bedside in the critically ill. If there is uncertainty about the results, esophagography can be performed. While this was traditionally performed via fluoroscopy, CT esophagography with contrast instilled either orally or via orogastric tube has shown some advantages (45,49). Low-osmolality water-soluble contrasts such as diatrizoate meglumine are the agents of choice. If no leak is identified, a follow-up image with barium is performed (49,56).
Tracheobronchial injuries are a rare finding carrying a high mortality rate and are often associated with a concomitant esophageal injury when they do occur (7). Clinical findings of tracheobronchial injury include subcutaneous emphysema, tachypnea, hoarseness, and hemoptysis (31,57,58). Pneumomediastinum and deep cervical emphysema are radiographic findings on CXR consistent with tracheobronchial injury (58-60). The endotracheal balloon may appear hyperinflated or malpositioned. Pneumothorax may be present if the injury is located distal to the mainstem bronchi. On CT, soft tissue emphysema extending into the lower chest wall and pneumomediastinum are suggestive findings (4,57,58). An angulated bronchus or bronchial defect may be detected on CT for bronchial injuries. The “fallen lung” sign is a radiographic finding that occurs in complete transection of the bronchus, causing the lung to deviate from the bronchus (2,4). Persistent subcutaneous emphysema, pneumothorax, or atelectasis on repeat CXR may raise the concern of an occult tracheobronchial injury. The gold standard for diagnosis of tracheobronchial injury is fiberoptic bronchoscopy (2).
Using a combination of these tests allows clinicians to assess the relevant structures in the mediastinum which, in turn, will guide operative management. Even in the stable patient work up should be conducted rapidly as delays in diagnosis and operative management have been linked to worse outcomes (50).
Conclusions
Transmediastinal penetrating trauma remains a difficult clinical challenge. A systematic approach in the emergency department to diagnosis and management should be undertaken and patients in extremis or with hemodynamic compromise rapidly identified. The unstable patient forgoes further investigations and the surgeon must use knowledge about the hypothesized trajectory, results of limited imaging, chest tube output, and anticipation of resuscitative maneuvers to select the best operative approach. In patients who are sufficiently stable to undergo CTA of the chest, the trajectory of the missile or impalement can often be seen and this is used to guide further investigation or operation. In those where ambiguity remains, more focused tests such as echocardiography, pericardial window, esophagoscopy or esophagography, and bronchoscopy can be used to assess the mediastinal structures. This tiered approach to stable patients helps avoid costly, timely, and often needless interventions and has been adopted by major trauma centers since the end of the 20th century (3,21-23).
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Simon R. Turner) for the series “Traumatic Injuries of the Mediastinum” published in Mediastinum. The article has undergone external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/med-21-14). The series “Traumatic Injuries of the Mediastinum” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Okoye OT, Talving P, Teixeira PG, et al. Transmediastinal gunshot wounds in a mature trauma centre: Changing perspectives. Injury 2013;44:1198-203. [Crossref] [PubMed]
- Gunn ML, Clark RT, Sadro CT, et al. Current concepts in imaging evaluation of penetrating transmediastinal injury. Radiographics 2014;34:1824-41. [Crossref] [PubMed]
- Renz BM, Cava RA, Feliciano DV, et al. Transmediastinal gunshot wounds: A prospective study. J Trauma 2000;48:416-21; discussion 421-2. [Crossref] [PubMed]
- Grossman MD, May AK, Schwab CW, et al. Determining anatomic injury with computed tomography in selected torso gunshot wounds. J Trauma 1998;45:446-56. [Crossref] [PubMed]
- Stassen NA, Lukan JK, Spain DA, et al. Reevaluation of diagnostic procedures for transmediastinal gunshot wounds. J Trauma 2002;53:635-8. [Crossref] [PubMed]
- Ivey KM, White CE, Wallum TE, et al. Thoracic injuries in US combat casualties: a 10-year review of Operation Enduring Freedom and Iraqi Freedom. J Trauma Acute Care Surg 2012;73:S514-S519. [Crossref] [PubMed]
- Burack JH, Kandil E, Sawas A, et al. Triage and outcome of patients with mediastinal penetrating trauma. Ann Thorac Surg 2007;83:377-82; discussion 382. [Crossref] [PubMed]
- Degiannis E, Benn C, Leandros E, et al. Transmediastinal gunshot injuries. Surgery 2000;128:54-8. [Crossref] [PubMed]
- Fowler KA, Dahlberg LL, Haileyesus T, et al. Firearm injuries in the United States. Prev Med 2015;79:5-14. [Crossref] [PubMed]
- Smith GA. Knife-related injuries treated in United States emergency departments, 1990-2008. J Emerg Med 2013;45:315-23. [Crossref] [PubMed]
- Demetriades D, Kimbrell B, Salim A, et al. Trauma deaths in a mature urban trauma system: is "trimodal" distribution a valid concept? J Am Coll Surg 2005;201:343-8. [Crossref] [PubMed]
- Davis JS, Satahoo SS, Butler FK, et al. An analysis of prehospital deaths: Who can we save? J Trauma Acute Care Surg 2014;77:213-8. [Crossref] [PubMed]
- Winfield RD, Crandall M, Williams BH, et al. Firearm violence in the USA: A frank discussion on an american public health crisis - the kansas city firearm violence symposium. Trauma Surg Acute Care Open 2019;4:e000359 [Crossref] [PubMed]
- Cornwell EE 3rd, Kennedy F, Ayad IA, et al. Transmediastinal gunshot wounds: A reconsideration of the role of aortography. Arch Surg 1996;131:949-52; discussion 952-3. [Crossref] [PubMed]
- Hanpeter DE, Demetriades D, Asensio JA, et al. Helical computed tomographic scan in the evaluation of mediastinal gunshot wounds. J Trauma 2000;49:689-94; discussion 694-5. [Crossref] [PubMed]
- Back MR, Baumgartner FJ, Klein SR. Detection and evaluation of aerodigestive tract injuries caused by cervical and transmediastinal gunshot wounds. J Trauma 1997;42:680-6. [Crossref] [PubMed]
- Ibirogba S, Nicol A, Navsaria P. Screening helical computed tomographic scanning in haemodynamic stable patients with transmediastinal gunshot wounds. Injury 2007;38:48-52. [Crossref] [PubMed]
- Singaravelu KP, Saya RP, Pandit VR. Early Diagnosis of Penetrating Cardiac and Pleural Injury by Extended Focused Assessment with Sonography for Trauma. Heart Views 2016;17:151-3. [Crossref] [PubMed]
- Galvagno SM Jr, Nahmias JT, Young DA. Advanced Trauma Life Support Update 2019: Management and Applications for Adults and Special Populations. Anesthesiol Clin 2019;37:13-32. [Crossref] [PubMed]
- Eastes LS, Norton R, Brand D, et al. Outcomes of patients using a tiered trauma response protocol. J Trauma 2001;50:908-13. [Crossref] [PubMed]
- Granström A, Strömmer L, Schandl A, et al. A criteria-directed protocol for in-hospital triage of trauma patients. Eur J Emerg Med 2018;25:25-31. [Crossref] [PubMed]
- Haider AA, Azim A, Rhee P, et al. Substituting systolic blood pressure with shock index in the National Trauma Triage Protocol. J Trauma Acute Care Surg 2016;81:1136-41. [Crossref] [PubMed]
- Joseph B, Khan M, Jehan F, et al. Improving survival after an emergency resuscitative thoracotomy: a 5-year review of the Trauma Quality Improvement Program. Trauma Surg Acute Care Open 2018;3:e000201 [Crossref] [PubMed]
- Panossian VS, Nederpelt CJ, El Hechi MW, et al. Emergency Resuscitative Thoracotomy: A Nationwide Analysis of Outcomes and Predictors of Futility. J Surg Res 2020;255:486-94. [Crossref] [PubMed]
- Meizoso JP, Ray JJ, Karcutskie CA 4th, et al. Effect of time to operation on mortality for hypotensive patients with gunshot wounds to the torso: The golden 10 minutes. J Trauma Acute Care Surg 2016;81:685-91. [Crossref] [PubMed]
- Bickell WH, Wall MJ Jr, Pepe PE, et al. Immediate versus delayed fluid resuscitation for hypotensive patients with penetrating torso injuries. N Engl J Med 1994;331:1105-9. [Crossref] [PubMed]
- Holcomb JB, Tilley BC, Baraniuk S, et al. Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma: the PROPPR randomized clinical trial. JAMA 2015;313:471-82. [Crossref] [PubMed]
- Meyer DE, Vincent LE, Fox EE, et al. Every minute counts: time to delivery of initial massive transfusion cooler and its impact on mortality. J Trauma Acute Care Surg 2017;83:19-24. [Crossref] [PubMed]
- Ditkofsky NG, Maresky H, Mathur S. Imaging Ballistic Injuries. Can Assoc Radiol J 2020;71:335-43. [Crossref] [PubMed]
- Dosios TJ, Salemis N, Angouras D, et al. Blunt and penetrating trauma of the thoracic aorta and aortic arch branches: an autopsy study. J Trauma 2000;49:696-703. [Crossref] [PubMed]
- Gunn ML. Imaging of aortic and branch vessel trauma. Radiol Clin North Am 2012;50:85-103. [Crossref] [PubMed]
- Huber-Wagner S, Lefering R, Qvick L, et al. Effect of whole-body CT during trauma resuscitation on survival: a retrospective, multicentre study. Lancet 2009;373:1455-61. [Crossref] [PubMed]
- Malhotra AK, Fabian TC, Croce MA, et al. Minimal aortic injury: a lesion associated with advancing diagnostic techniques. J Trauma 2001;51:1042-8. [Crossref] [PubMed]
- O'Connor JV, Scalea TM. Penetrating thoracic great vessel injury: impact of admission hemodynamics and preoperative imaging. J Trauma 2010;68:834-7. [Crossref] [PubMed]
- Plurad DS, Bricker S, Van Natta TL, et al. Penetrating cardiac injury and the significance of chest computed tomography findings. Emerg Radiol 2013;20:279-84. [Crossref] [PubMed]
- Karrel R, Shaffer M, Franaszek J. Emergency diagnosis, resuscitation, and treatment of acute penetrating cardiac trauma. Ann Emerg Med 1982;11:504-17. [Crossref] [PubMed]
- Wu Y, Qamar S, Murray N, et al. Imaging of Cardiac Trauma. Radiol Clin North Am 2019;57:795-808. [Crossref] [PubMed]
- Saranteas T, Mavrogenis A, Mandila C, et al. Ultrasound in cardiac trauma. J Crit Care 2017;38:144-51. [Crossref] [PubMed]
- Rozycki GS, Feliciano DV, Ochsner MG, et al. The role of ultrasound in patients with possible penetrating cardiac wounds: a prospective multicenter study. J Trauma 1999;46:543-51; discussion 551-2. [Crossref] [PubMed]
- Manzano-Nunez R, Gomez A, Espitia D, et al. A meta-analysis of the diagnostic accuracy of chest ultrasound for the diagnosis of occult penetrating cardiac injuries in hemodynamically stable patients with penetrating thoracic trauma. J Trauma Acute Care Surg 2021;90:388-95. [Crossref] [PubMed]
- Ball CG, Williams BH, Wyrzykowski AD, et al. A caveat to the performance of pericardial ultrasound in patients with penetrating cardiac wounds. J Trauma 2009;67:1123-4. [Crossref] [PubMed]
- Restrepo CS, Gutierrez FR, Marmol-Velez JA, et al. Imaging patients with cardiac trauma. Radiographics 2012;32:633-49. Erratum in: Radiographics 2012;32:1258. [Crossref] [PubMed]
- Goldstein L, Mirvis S, Kostrubiak I, et al. CT diagnosis of acute pericardial tamponade after blunt chest trauma. AJR Am J Roentgenol 1989;152:739-41. [Crossref] [PubMed]
- Shimoyamada K, Yamaguchi T, Hayakawa M, et al. Significance of incidental pericardial effusion on computed tomography in cardiac trauma: a report of two cases. Emerg Radiol 1996;3:130-3. [Crossref]
- Krejci CS, Blackmore CC, Nathens A. Hemopericardium: an emergent finding in a case of blunt cardiac injury. AJR Am J Roentgenol 2000;175:250. [Crossref] [PubMed]
- Restrepo CS, Lemos DF, Lemos JA, et al. Imaging findings in cardiac tamponade with emphasis on CT. RadioGraphics 2007;27:1595-610. [Crossref] [PubMed]
- LeBlang SD, Dolich MO. Imaging of penetrating thoracic trauma. J Thorac Imaging 2000;15:128-35. [Crossref] [PubMed]
- Shanmuganathan K, Matsumoto J. Imaging of penetrating chest trauma. Radiol Clin North Am 2006;44:225-38. [Crossref] [PubMed]
- Arantes V, Campolina C, Valerio S, et al. Flexible esophagoscopy as a diagnostic tool for traumatic esophageal injuries. J Trauma 2009;66:1677-82. [Crossref] [PubMed]
- Ahmed N, Massier C, Tassie J, et al. Diagnosis of penetrating injuries of the pharynx and esophagus in the severely injured patient. J Trauma 2009;67:152-4. [Crossref] [PubMed]
- Swanson JO, Levine MS, Redfern RO, et al. Usefulness of high-density barium for detection of leaks after esophagogastrectomy, total gastrectomy, and total laryngectomy. AJR Am J Roentgenol 2003;181:415-20. [Crossref] [PubMed]
- Fadoo F, Ruiz D, Dawn S, et al. Helical CT esophagography for the evaluation of suspected esophageal perforation or rupture. AJR Am J Roentgenol 2004;182:1177-9. [Crossref] [PubMed]
- Srinivasan R, Haywood T, Horwitz B, et al. Role of flexible endoscopy in the evaluation of possible esophageal trauma after penetrating injuries. Am J Gastroenterol 2000;95:1725-9. [Crossref] [PubMed]
- Biffl WL, Moore EE, Feliciano DV, et al. Western Trauma Association Critical Decisions in Trauma: Diagnosis and management of esophageal injuries. J Trauma Acute Care Surg 2015;79:1089-95. [Crossref] [PubMed]
- Asensio JA, Chahwan S, Forno W, et al. American Association for the Surgery of Trauma. Penetrating esophageal injuries: multicenter study of the American Association for the Surgery of Trauma. J Trauma 2001;50:289-96. [Crossref] [PubMed]
- Buecker A, Wein B, Neuerburg J, et al. Esophageal perforation: comparison of use of aqueous and barium-containing contrast media. Radiology 1997;202:683-6. [Crossref] [PubMed]
- Inaba K, Branco B, Menaker J, et al. Evaluation of multidetector computed tomography for penetrating neck injury: a prospective multicenter study. J Trauma Acute Care Surg 2012;72:576-83. [Crossref] [PubMed]
- Unger JM, Schuchmann GG, Grossman JE, et al. Tears of the trachea and main bronchi caused by blunt trauma: radiologic findings. AJR Am J Roentgenol 1989;153:1175-80. [Crossref] [PubMed]
- Johnson SB. Tracheobronchial injury. Semin Thorac Cardiovasc Surg 2008;20:52-7. [Crossref] [PubMed]
- Stark P. Imaging of tracheobronchial injuries. J Thorac Imaging 1995;10:206-19. [Crossref] [PubMed]
Cite this article as: Jogiat UM, Strickland M. Transmediastinal penetrating trauma. Mediastinum 2021;5:25.