
Type A thymoma invading the trachea: a case report
Introduction
Thymomas are the most common primary tumors of the anterior mediastinum (1). Generally they are indolent tumors but occasionally may show malignant behavior, by invading adjacent organs (2). According to the WHO classification thymomas are divided in five subtypes (A, AB, B1, B2, B3) based on the morphology of epithelial cells and the amount of lymphocytic component (3). Type A thymomas are diagnosed at an early stage in over 90% of cases and are characterized by a 10-year survival rate close to 100% (4).
Few cases of thymoma with endobronchial growth have been described and the only reported patient with tracheal invasion had a B3 thymoma (5). We present a typical type A thymoma with polypoid endotracheal growth, almost completely obstructing the airway.
We present the following article in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/med-20-63).
Case presentation
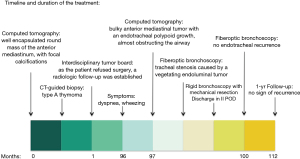
In April 2019 a 93-year-old man was referred to our hospital with severe dyspnea and wheezing from at least 5 weeks. Comorbidities: previous Legionella pneumonia; several episodes of colonic diverticulitis; benign prostatic hyperplasia. The patient was non-smoker, with an 8-year history of type A thymoma, discovered occasionally, and diagnosed by means of percutaneous core-needle biopsy. At the time of diagnosis, the computed tomography (CT) scan revealed a well encapsulated round mass of the anterior mediastinum, measuring 55×58×44 mm with focal calcifications (Figure 1A). As the patient refused surgery and radiation therapy, a follow-up with a yearly CT scan was scheduled, showing slow-growing disease until the last exam of February 2018, which revealed tracheal compression without any sign of invasion.
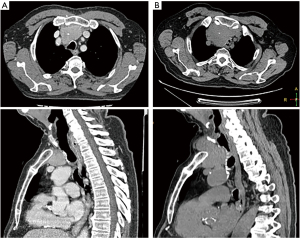
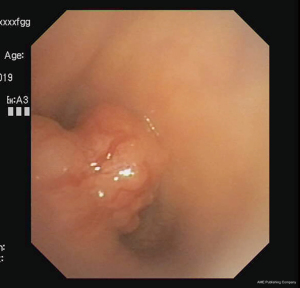
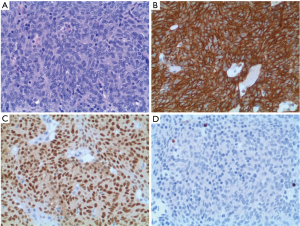
At the physical examination inspiratory stridor and tachypnea were recorded. Blood exams were in the normal range. The CT scan of the thorax revealed a bulky anterior mediastinal tumor with an endotracheal polypoid growth, almost obstructing the airway (Figure 1B). At the fiberoptic bronchoscopy we observed a severe tracheal stenosis caused by a vegetating endoluminal tumor with a mild extrinsic compression (Figure 2). An emergency rigid bronchoscopy, aimed to relieve the upper airway obstruction, was performed. Because of the critical airway obstruction, in order to facilitate the intraoperative conduct, we used an original alternative method for airway management with combined tracheal intubation and rigid bronchoscope (6).The endotracheal tumor had a relatively small base of implant and was totally removed with mechanical resection, using an 8.5 mm Storz ventilating rigid bronchoscope. Tissue fragments were entirely composed by a proliferation of oval or spindle neoplastic cells with bland nuclei and inconspicuous nucleoli, arranged in a fascicular pattern. Very few immature lymphocytes were present throughout the tumor. Immunohistochemical analysis showed a positive expression in neoplastic cells for pankeratin, paired-box gene 8 (PAX8), cytokeratin 19, cytokeratin 7, p63 and p40 and negativity for CD5, CD117 and CD20. Immature lymphocytes resulted positive for terminal deoxynucleotidyl transferase (TdT) (Figure 3).
Postoperative course was uneventful and the patient was discharged on postoperative day 2, without respiratory symptoms. The fiberoptic bronchoscopy, carried out 3 months after surgery, was negative for endotracheal recurrence. Due to his old age, the patient refused to perform any follow-up radiologic exam. Thus, follow-up was based on clinical evaluation and the patient is alive, without any respiratory symptom, 15 months after rigid bronchoscopy. Figure 4 displays the timeline for clinical presentation, diagnosis of thymoma invading the trachea, surgery and follow-up.
Written informed consent was obtained from the patient. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committees and with the Helsinki Declaration (as revised in 2013).
Discussion
Thymomas natural history entails a wide variety of biological behaviors. Most patients are asymptomatic or have a parathymic syndrome; symptoms related to invasion of mediastinal structures are sporadically reported, while clinical emergencies caused by thymomas are extremely rare (7). These tumors generally grow applying pressure to the adjacent organs but they may infiltrate the capsule and extend directly to them. The invasion of the airway is very rare (5). In the English Literature 21 cases of endobronchial growth are reported and most of them involved the left bronchial tree (5,8). Prior to the herein reported case, only one patient with endotracheal polypoid growth by an invasive B3 thymoma had been described (5).
Contrast CT of the thorax is the gold standard for the diagnosis of mediastinal masses and bronchoscopy is indicated only when the involvement of the airway is suspected (1). In previous reports, biopsies through a flexible bronchoscope have been attempted, resulting non-diagnostic in most cases (5,8). In the reported case, flexible bronchoscopy was performed in order to define the involvement of the tracheal wall and the residual respiratory space but, since the patient was highly symptomatic and the tracheal obstruction was severe, no biopsies were taken during such procedure. The emergency rigid bronchoscopy allowed to achieve both histology and palliation. Radical resection, stage and histotype are strong prognostic factors for thymoma patients (9). Surgery is the mainstay of treatment for most thymomas, while irradiation and chemotherapy are commonly administered to not-resectable tumors or in adjuvant regimens (1). Furthermore, surgery, as part of multimodality therapy, could prolong survival also for advanced stage thymomas (10). Our patient had been diagnosed with resectable type A thymoma, 8 years earlier, but he refused surgery; because of the low effectiveness of irradiation and chemotherapy on low-grade thymomas, a strict follow-up had been established. The tumor remained substantially stable for long time and eventually it invaded the tracheal wall growing inside the lumen. The slow growth of the tumor and the small implant base of the endotracheal growth have made the endoscopic palliative treatment performed effective and lasting, so far avoiding the use of stents or laser treatments.
Although type A thymomas are generally considered slow-growing tumors they cannot be defined as benign; some studies indeed have demonstrated invasive growth and distant metastases (4). Furthermore, a new entity of type A thymoma with atypical morphological features invading adjacent organs or spreading outside the chest has been recognized by the WHO classification (3). However, our patient was affected by a type A thymoma without any atypical feature, since no necrosis, atypia and mitotic activity were observed.
In conclusion, conservative treatment of typical type A thymoma in very elderly patients may be acceptable but careful follow-up, aimed to rule out a possible invasive growth, should be carried out.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/med-20-63
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/med-20-63). The authors have no conflicts of interest to declare.
Ethical statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patient. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committees and with the Helsinki Declaration (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Girard N, Ruffini E, Marx A, et al. Thymic epithelial tumours: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2015;26:v40-55. [Crossref] [PubMed]
- Tassi V, Vannucci J, Ceccarelli S, et al. Stage-related outcome for thymic epithelial tumours. BMC Surg 2019;18:114. [Crossref] [PubMed]
- Marx A, Ströbel P, Badve SS, et al. ITMIG consensus statement on the use of the WHO histological classification of thymoma and thymic carcinoma: refined definitions, histological criteria, and reporting. J Thorac Oncol 2014;9:596-611. [Crossref] [PubMed]
- Vladislav IT, Gökmen-Polar Y, Kesler KA, et al. The role of histology in predicting recurrence of type A thymomas: a clinicopathologic correlation of 23 cases. Mod Pathol 2013;26:1059-64. [Crossref] [PubMed]
- Hwang JT, Kim MH, Chang KJ, et al. A case of invasive thymoma with endotracheal polypoid growth. Tuberc Respir Dis (Seoul) 2012;73:331-5. [Crossref] [PubMed]
- Puma F, Meattelli M, Kolodziejek M, et al. An alternative method for airway management with combined tracheal intubation and rigid bronchoscope. Ann Thorac Surg 2019;107:e435-6. [Crossref] [PubMed]
- Santoprete S, Ragusa M, Urbani M, et al. Shock induced by spontaneous rupture of a giant thymoma. Ann Thorac Surg 2007;83:1526-8. [Crossref] [PubMed]
- Zhang R, Li J, Zhang H A. "coughed up" tissue diagnosed as type A thymoma in an 80-year-old man: a case report. Medicine (Baltimore) 2019;98:e16337. [Crossref] [PubMed]
- Tassi V, Ceccarelli S, Zannori C, et al. Could thymomectomy be a reasonable option for non-myasthenic thymoma patients? J Thorac Dis 2017;9:3817-24. [Crossref] [PubMed]
- Fiorelli A, D'Andrilli A, Vanni C, et al. Iterative surgical treatment for repeated recurrences after complete resection of thymic tumors. Ann Thorac Surg 2017;103:422-31. [Crossref] [PubMed]
Cite this article as: Tassi V, Puma F, Bellezza G, Ceccarelli S. Type A thymoma invading the trachea: a case report. Mediastinum 2021;5:36.


