
Spontaneous mediastinal emphysema in a non-intubated patient with COVID-19 related pneumonia: a case report
Introduction
Recently due to the SARS-CoV-2 viral pandemic a surge in related hospital admissions have presented globally. Mediastinal emphysema (ME) is a complication that rarely presents in non-ventilated patients (1,2). Thus, we describe a case of a patient with isolated pneumomediastinum (ME without pneumothorax) in the context of COVID-19 related pneumonia that was treated conservatively with complete resolution of symptoms. We present the following case in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/med-21-5).
Case presentation
A 58-year-old man with unremarkable past medical history presented to the emergency department with 7 days of marked dyspnea, cough, perception of enlarged neck’s circumference, crepitus and dysphagia. Previously, he received treatment with azithromycin and dexamethasone every 24 hours during 5 days as an outpatient, with no improvement. He did suspect recent coronavirus exposure. He denied smoking history, alcohol or drug usage. On admission his vital signs showed tachypnea (25 breaths per minute), increased heart rate (105 beats per minute), low grade fever (38.1 °C) and oxygen saturation of 87% on room air, improving to 95% on 15 L/min non-rebreather mask. On examination, he had shortness of breath without the use of accessory muscles. During examination, he was noted to have crepitus around his neck, anterior chest area and around the submandibular space. The auscultation revealed bilateral basal crackles; a Hamman sign was audible. Laboratory results showed an elevated C-reactive protein (CRP) of 3.66 mg/dL (normal range, 0–0.50 mg/dL), ferritin 577 ng/mL (normal range, 23–336.2 ng/mL), D-dimer 800 ng/mL (normal range, 0–500 ng/mL) and lymphopenia 235 cells/field. His arterial blood gas levels revealed a respiratory insufficiency type 1 and a respiratory alkalosis with pH of 7.54, partial pressure of carbon dioxide (pCO2) of 26.3 mmHg, pO2 of 54 mmHg, HCO3 22 mmol/L, lactate 1.3 mmol/L on supplementary oxygen with nasal canula (4 L/min) and a calculated PaO2/FiO2 ratio of 145.
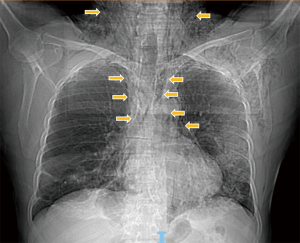
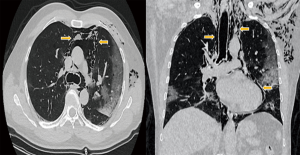
A chest X-ray was performed showing bilateral ground-glass opacities and diffuse infiltrates at the bilateral lung bases, as well as evidence of subcutaneous emphysema (Figure 1). Non-contrast chest computed tomography (CT) showed ground-glass opacities with peripheral subpleural location associated with areas of consolidation in posterolateral segments of both lower lobes, a pattern compatible with COVID-19. Pneumomediastinum with extension to the subcutaneous soft tissues of the left hemithorax and neck up to the skull base and submandibular space was also observed (Figure 2) reverse transcription (RT)-PCR analysis of COVID-19 resulted positive. The patient was started on dexamethasone 6 mg intravenously and low molecular weight heparin 0.6 mg daily for thromboprophylaxis remaining stable with non-invasive supplemental oxygen without any related adverse effect. Unfortunately, remdesivir was not available at that moment at our center due to issues related with chain supply. His extensive pneumomediastinum was managed conservatively and monitored by daily chest X-ray where gradual improvement was observed. On 72 hours following admission, a subsequent chest CT-scan demonstrated significant decrease in pneumomediastinum and pneumonia with slight radiological improvement. Subsequently, the radiological follow-up demonstrated complete resolution of ME. The patient was discharged completely asymptomatic on day 10 after admission.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). A written consent has been obtained from the patient.
Discussion
During the SARS-CoV-2 pandemic an increased frequency of air leaks, spontaneous pneumothorax and ME has been reported even in patients without mechanical ventilation or in the absence of another predisposing factors (1,2). Other than COVID-19 related pneumonia the patient presented in this case, reported with no significant risk factors neither a primary pulmonary condition associated with ME. The primary radiologic evaluation of the patient showed no bullae, cyst or associated pneumothorax. The presence of ME in the context of viral associated pneumonia has been proposed as a clinical feature related with poor prognosis, even with increased risk of intubation and morbidity (1,3). Fortunately, in this case the patient had complete resolution of symptoms requiring only conservative management.
The pathophysiology underlying this presentation is not completely understood and requires further research to elucidate. Notably, the presence of ME has been previously reported in association with viral respiratory infections (4,5). The distinguished affection of pulmonary parenchyma putatively caused by SARS-CoV-2 infection has been linked with the presence of diffuse alveolar rupture and unusual patterns of vascular angiogenesis that may predispose to these complications (6,7). Another predisposing factor inducing increased airway pressures in these patients is the presence of pronounced cough that generates a Macklin-like effect, a proposed mechanism of pneumomediastinum that involves alveolar rupture with the consequent dissection of free air along the peribronchovascular interstitial sheaths and in to the visceral pleura of the mediastinum (8).
We aim to emphasize that even though only non-invasive maneuvers are required for the management of most cases with ME. Monitorization of patients assessing for any sign of sudden clinical deterioration is valuable in order to timely recognize and attend life threatening complications in which surgical decompression could be needed. Rarely pneumopericardium have also been reported (9,10). The long-term prognosis of patients with complete resolution of ME in the context of COVID-19 related pneumonia is uncertain. Thus, sequential follow up after discharge could be rational.
The patient shared the following thoughts on his experience during pre-admission and management: “I was surprised when dyspnea and coughing appeared, however I did not think at all that it was COVID-19. The shortness of breath and the neck enlargement were my main concern when I presented to the emergency department. That growth came on suddenly, even though I was already receiving treatment. Doctors told me that if the disease worsened, intubation was necessary and if the air in the neck did not disappear, some surgical treatment would be considered. They gave me oxygen in a non-rebreather mask. I was worried about everything, not having a clue of how many days and how many nights I would be there. The doctors told me that subsequent chest x-ray images showed improvement of the pneumonia without any subcutaneous emphysema visible. I felt better as the days went by.”.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/med-21-5
Peer Review File: Available at http://dx.doi.org/10.21037/med-21-5
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/med-21-5). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). A written consent has been obtained from the patient.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Manna S, Maron SZ, Cedillo MA, et al. Spontaneous subcutaneous emphysema and pneumomediastinum in non-intubated patients with COVID-19. Clin Imaging 2020;67:207-13. [Crossref] [PubMed]
- Eperjesiova B, Hart E, Shokr M, et al. Spontaneous pneumomediastinum/pneumothorax in patients with COVID-19. Cureus 2020;12:e8996 [Crossref] [PubMed]
- Chu CM, Leung YY, Hui JY, et al. Spontaneous pneumomediastinum in patients with severe acute respiratory syndrome. Eur Respir J 2004;23:802-4. [Crossref] [PubMed]
- Silva C, Almeida AF, Ferraz C, et al. Spontaneous pneumothorax with subcutaneous emphysema: a rare complication of respiratory syncytial virus infection. J Clin Med Res 2016;8:260-2. [Crossref] [PubMed]
- Essa RA, Al-Helali I, Al-Benhassan I, et al. Subcutaneous emphysema and pneumomediastinum secondary to H1N1 pneumonia in Saudi children: 2 case reports. Curr Pediatr Res 2017;21:301-5.
- Ackermann M, Verleden SE, Kuehnel M, et al. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid-19. N Engl J Med 2020;383:120-8. [Crossref] [PubMed]
- Kommoss FKF, Schwab C, Tavernar L, et al. The pathology of severe COVID-19-related lung damage. Dtsch Arztebl Int 2020;117:500-6. [PubMed]
- Macklin MT, Macklin CC. Malignant interstitial emphysema of the lungs and mediastinum as an important occult complication in many respiratory diseases and other conditions: An interpretation of the clinical literature in the light of laboratory experiment. Medicine 1944;23:281-358. [Crossref]
- Sahu KK, Mishra AK, Goldman Y. A rare case of pneumopericardium secondary to COVID-19. Heart Lung 2020;49:679-80. [Crossref] [PubMed]
- Ghods K, Aghaamoo S, Amini Fooladi N, et al. Spontaneous massive pneumopericardium in a patient with COVID-19. Eur J Cardiothorac Surg 2020; Epub ahead of print. [Crossref] [PubMed]
Cite this article as: Armillas-Canseco F, León-Cabral P, Tello-Mercado AC, Gomez-Portugal EP. Spontaneous mediastinal emphysema in a non-intubated patient with COVID-19 related pneumonia: a case report. Mediastinum 2021;5:20.


