
Large mediastinal schwannoma with great vessel encroachment requiring vascular reconstruction: a case report
Introduction
In the posterior mediastinum, the most common tumor is of neurogenic origin, composing of 12.0–39.0% of all mediastinal tumors (1). The majority of these tumors are benign peripheral nerve sheath tumors (PNST), such as schwannomas, and account for approximately 95% of all neurogenic tumors (1-3). Schwannomas are usually asymptomatic, solitary masses and are benign and approximately two thirds of cases. However, when symptoms do occur, they are often due to involvement and compression of neighboring structures and carry a greater risk of being malignant (2). Due to the indolent nature of the tumor, schwannomas have the potential to grow large and encase and invade important anatomical surrounding structures, such as the aorta, pulmonary vessels, and left subclavian and innominate arteries, which could lead to catastrophic consequences (4). This is a case of a large mediastinal schwannoma with significant involvement of the aortic arch requiring extensive surgical resection and vascular reconstruction. We present the following case in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/med-20-71).
Case presentation
A 73-year-old male initially presented to his primary physician with a persistent cough, but denied dysphagia or dyspnea. His workup included chest radiography and a subsequent chest computed tomography (CT) which demonstrated a 7.2 cm mediastinal mass. Percutaneous biopsy of the mass was reported as consistent with schwannoma. Further chest CT angiography (CTA) demonstrated a 6.3×5.7×11.5 cm3 mass in the posterior superior mediastinum between the trachea and left subclavian artery, abutting the aortic arch, with mass effect on the trachea and esophagus (Figures 1,2).

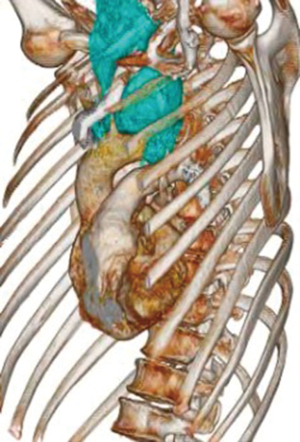
After a multidisciplinary tumor board discussion, the decision was to proceed with surgical resection given the tumor size, location, and concern for continued progression which could lead to additional compression of the esophagus, trachea, or aortic arch, with associated catastrophic consequences. Since the tumor encased the subclavian and vertebral arteries, pre-operative planning included consideration for vascular surgery involvement. However, given the nature and imaging characteristics, concern for aortic reconstruction and cardiopulmonary bypass was not deemed necessary. On 9/15/20, the patient underwent a bronchoscopy, left trapdoor incision (left supraclavicular incision, median sternotomy, left anterolateral thoracotomy), partial thymectomy, mediastinal dissection and excision of mediastinal tumor. While tumor appeared encapsulated, it was adherent to the posterior aortic arch, encasing the vertebral and left subclavian artery. These findings were evaluated by two vascular surgeons who assisted with the dissection of the tumor off the aortic arch. Tumor resection without capsule violation required excision of a segment of the left subclavian artery at the bifurcation of the vertebral artery. An interposition polytetrafluoroethylene (PTFE) graft was used to revascularize the left subclavian artery and the left vertebral artery was reimplanted onto native subclavian artery. The patient recovered well from surgery without postoperative complications and was discharged home on postoperative day four.
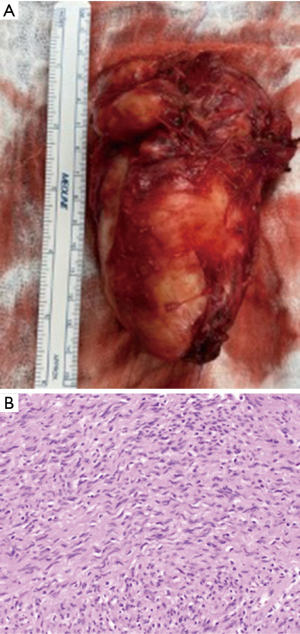
Final pathology revealed two separate Schwannomas, one 11 cm, the other 3.5 cm, each completely excised with negative margins, with 45 benign lymph nodes (Figure 3). On post-operative follow up, the patient endorsed resolution of his prior cough, however continued to have persistent hoarseness, which subsequently resolved with time.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Discussion
Schwannomas, also known as neurilemmomas, are usually benign, well-encapsulated tumors arising from neural crest cells, Schwann cells, of neural sheath origin (5). While multiple Schwannomas arising from a single nerve have been described, these tumors typically arise from the sympathetic chain or an intercostal nerve. There have also been several reports in the literature of tumors originating from the vagus or recurrent laryngeal nerves (6,7).
Given the initial asymptomatic course, most mediastinal tumors are found incidentally and the diagnosis of a schwannoma can be suggested by certain CT and magnetic resonance imaging (MRI) characteristics. A typical CT may elucidate a homogenous, low attenuation lesion (3). Mediastinal schwannomas range in size from 2 to 10 cm, although can exceed this range, further demonstrating the wide scope of anatomical structures which can potentially be involved and invaded (3).
Management of mediastinal schwannomas is guided by several factors, which includes clinical presentation and symptoms, tumor size, location, complications due to tumor growth, and pathology (8). Schwannomas tend to grow slowly and can have a long indolent course, therefore small, asymptomatic, incidentally found mediastinal schwannomas can be observed with serial imaging to monitor progression (9). However, given the propensity for the mediastinal tumor to continue to grow and potentially invade surrounding structures, the treatment of choice is surgical resection of the mass, either by video assisted thoracoscopy or thoracotomy, for definitive diagnosis and treatment (3,6,10). Ultimately, prognosis is excellent as benign schwannomas rarely recur (2).
Surgical approach must take into consideration the location of the tumor, structures involved and surgeon experience and minimally invasive and open techniques (2). Mediastinal tumors, including schwannomas, can often be approached with minimally invasive and robotic techniques. As a high volume robotic thoracic center, about 15% of our minimally invasive cases consist of mediastinal tumor resections. We have previously described the feasibility of robotic resection for paravertebral schwannomas in challenging locations such as the superior sulcus (11).In contrast, this case report from our center demonstrates successful collaborative management of a rare complex mediastinal schwannoma. Open resection and vascular reconstruction were required to ensure complete removal of the tumor.
There have been previous reports of large schwannomas abutting adjacent structures. These cases have included involvement of the surrounding pulmonary parenchyma causing hemoptysis, aortic and pulmonary artery involvement, as well as a case of a malignant schwannoma invading the thoracic aorta, leading to pathologic aortic rupture and catastrophic hemorrhage (4,7,12). To our best knowledge, this is the first case report which describes a mediastinal schwannoma with extensive involvement of the aortic arch, requiring vascular surgery involvement and subclavian interposition bypass. This case further highlights the nature of the tumor, as it often progresses undetected for prolonged periods of time due to its asymptomatic course, allowing time for the tumor to become quite large, encase surrounding structures. Due to the anatomical significance of these structures in the mediastinum, the consequences can be impressive, requiring extensive surgical resection and at times involvement of multiple surgical specialties during the index operation.
Given the propensity of the tumor to grow undetected for extensive periods of time, thorough evaluation of the tumor with imaging allows for preoperative planning to perform the optimal surgical resection with all necessary surgical specialties providing the best approach and resection possible.
Acknowledgments
The authors would like to thank Michael Fuentes and Octavio Jose Redondo in the August 2020 to July 2022 at the University of Miami for their assistance in creating 3D reconstructed images used in this case report.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/med-20-71
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/med-20-71). Dr. NRV serves as an unpaid editorial board member from Department of Radiology. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Erickson LA. Posterior Mediastinal Schwannoma (Neurilemmoma). Mayo Clin Proc 2019;94:559-60. [Crossref] [PubMed]
- Dy P, Lajom C, Sanchez J. Middle mediastinal schwannoma concealed by asthma and GORD. BMJ Case Rep 2018;2018:bcr2017223795. [Crossref] [PubMed]
- Wu Y, Zhang J, Chai Y. Giant mediastinal schwannoma located in the lower right side of the chest. Niger J Clin Pract 2016;19:678-80. [Crossref] [PubMed]
- Bambirra EA, Miranda D. Spontaneous aortic rupture in a malignant schwannoma. South Med J 1980;73:1533-5. [Crossref] [PubMed]
- Gueldich M, Hentati A, Chakroun A, et al. Giant cystic schwannoma of the middle mediastinum with cervical extension. Libyan J Med 2015;10:27409. [Crossref]
- Fierro N, D'ermo G, Di Cola G, et al. Posterior mediastinal schwannoma. Asian Cardiovasc Thorac Ann 2003;11:72-3. [Crossref] [PubMed]
- Das A, Choudhury S, Basuthakur S, et al. Massive hemoptysis: a rare presentation of posterior mediastinal, giant, benign vagal schwannoma. Arch Iran Med 2014;17:779-82. [PubMed]
- Souza LCA, Pinto TDA, Cavalcanti HOF, et al. Esophageal schwannoma: Case report and epidemiological, clinical, surgical and immunopathological analysis. Int J Surg Case Rep 2019;55:69-75. [Crossref] [PubMed]
- Zarei S, Popa A, Moghadam B, et al. Oversized primary intrapulmonary schwannoma: A case report and a review of the literature. Surg Neurol Int 2020;11:234. [Crossref] [PubMed]
- Loftus TJ, Pipkin M, Machuca T, et al. Angiographic embolization followed by piecemeal resection of giant posterior mediastinal schwannoma: Case report and concise review. Int J Surg Case Rep 2018;53:250-3. [Crossref] [PubMed]
- Pacchiarotti G, Wang MY, Kolcun JPG, et al. Robotic paravertebral schwannoma resection at extreme locations of the thoracic cavity. Neurosurg Focus 2017;42:E17. [Crossref] [PubMed]
- Ito Y, Tanaka N. Mediastinal neurinoma originating from the intrathoracic vagal nerve: report of a case. Kyobu Geka 2009;62:513-5. [PubMed]
Cite this article as: Szewczyk JB, Hachey K, Rey J, Nguyen DM, Villamizar NR. Large mediastinal schwannoma with great vessel encroachment requiring vascular reconstruction: a case report. Mediastinum 2021;5:37.


