
Comparison of surgical outcomes after robotic assisted thoracic surgery, video-assisted thoracic surgery and open resection of thymoma
Introduction
Thymomas are the most common neoplasm in the anterior mediastinum and represent 20% of all neoplasms in the anterior mediastinum among adults (1). Thymomas are associated with several paraneoplastic conditions whereas myasthenia gravis is the most common syndrome associated with thymoma (2). Thymomas are traditionally staged by the Masaoka Koga staging system (3), but in addition, the international committee of the World Health Organization (WHO) has established a histopathological classification system for thymomas based on the morphology of the epithelial cells and the ratio between lymphocytic and epithelial cells (4). However, the Masaoka Koga staging system remains the most frequently applied system for staging thymomas (5).
Long-term survival from thymoma depends on the stage, whereas stage I and type A are associated with a survival rate from 80% to 90% (2,3,6). Surgical treatment remains the only curative treatment and if R0-resection is achieved through surgery (7,8), resection is associated with higher long-term survival compared to subtotal resection (3). Traditionally the surgery has been performed through median sternotomy. Minimal invasive surgery through unilateral thoracoscopy has shown its benefits compared to open surgery, in regards of postoperative recovery. Modern robots can be used to improve surgical outcomes and precision of the resection. However, the evidence regarding robotic assisted resection of thymomas is very sparse, and primarily being compared to open surgery (9,10). We present the following article in accordance with the Transparent Reporting of Evaluations with Nonrandomized Designs (TREND) reporting checklist (available at http://dx.doi.org/10.21037/med-20-56).
The aim of this retrospective study was to investigate the impact of the surgical approach on morbidity and length of stay for patients treated surgically for thymomas comparing three surgical techniques.
Methods
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional board of Odense University Hospital, Denmark with case number 17/44005 as a retrospective quality control study without need for informed consent from the patients.
Data extraction
Data from a single center database were extracted throughout the period from 01 January 2006 until 01 January 2019. Patients with Masoka stage I and II thymoma were suitable for surgical thymectomy at our clinic. Treatment of patients with Masoka stage III and IV has been centralized at Rigshospitalet, Copenhagen in Denmark and are not included in this study. A few number of patients were treated surgically for stage III thymoma at our clinic in cases where the stage was not known prior to surgery but were referred to Rigshospitalet, Denmark for further oncological treatment and follow-up. A total number of 80 patients were identified. We retrospectively reviewed medical records of all patients who underwent surgical complete thymectomy in compliance with General Data Protection Regulation law.
Inclusion criteria
All patients that underwent surgical thymectomy from 01 January 2006 until 01 January 2019.
Exclusion criteria
Patients with invasion in great vessels, thoracic wall and disseminated disease.
Data analysis
Microsoft Excel and STATA was used to process the extracted data. Demographic characteristics were summarized by standard descriptive summaries, with mean or median and standard deviation or Interquartile range for continues variables such as age. Categorical variables such as gender were presented in percentages.
For nominal variables, a Kruskal-Wallis test was performed, which was followed by a post-hoc Mann-Whitney test if there was any significant difference. For continues variables, that was assumed normally distributed a one-sided analysis of variance (ANOVA) test was applied. If the ANOVA test showed a significant difference within the groups, a post-hoc two-sided t-test was performed. The correlating P value were identified.
If the one-sided ANOVA test demonstrated no significant difference between groups, the P value of the ANOVA test would be presented.
P<0.05 was set as statistical significance level.
Surgical techniques
The surgical approach has changed throughout the inclusion time in this study. In 2006, the patients were treated through open surgery until the shift towards minimal invasive surgery and finally to robotic assisted surgery.
Robotic-assisted thoracoscopic surgery (RATS)
The Intuitive DaVinci robot was used to perform the RATS surgery. The robotic procedure was performed through four lateral port incisions under CO2 insufflation, double lumen intubation and intercostal blockades. One port was for the thoracoscope, two ports for the robotic arms and the last port was a utility port for the assistant. The anterior mediastinum was entered through the pleura from one side and the thymus was dissected and removed in toto in an endobag through the utility port. The phrenic nerve was visualized on both sides and spared. All patients had one chest tube which was removed after mobilization of the patient. All patients were started in oral analgesics for 2 weeks the day of surgery (paracetamol and long-acting opioids).
Video-assisted thoracoscopic surgery (VATS)
The VATS procedure was performed through 3 lateral port incisions under CO2 insufflation, double lumen intubation and intercostal blockades. One port is for the thoracoscope while the other two were for surgical instruments. The anterior mediastinum was entered through the pleura from one side and the thymus was dissected and removed in toto in an endobag through the utility port. The phrenic nerve was visualized on both sides and spared. All patients had one chest tube which was removed after mobilization of the patient. All patients were started in oral analgesics for 2 weeks the day of surgery (paracetamol and long-acting opioids).
Open surgery
The anterior mediastinum was mostly accessed through sternotomy, but in some cases, through a thoracotomy. Both procedures were performed with double lumen intubation and epidural catheter (EPI). After entering the anterior mediastinum, the thymus was dissected, resected and removed. The phrenic nerve was visualized on both sides and spared. All patients had one chest tube which was removed after mobilization of the patient. All patients were started in oral analgesics [nonsteroidal anti-inflammatory drug (NSAID), paracetamol and long-acting opioids] for 3 weeks after removal of the chest tube. The EPI would routinely be removed after chest tube removal except in cases with prolonged time with chest tube.
Postoperative treatment
The resected thymus was marked intraoperatively according to the International Thymic Malignancy Interest Group (ITMIG) guideline (11). If the radically was not secured macroscopically, the area of uncertainty would be marked. The Masaoka Koga staging was used as staging system due to its frequent use and the stage determined by a pathologist. Patients with Masoka stage II thymomas without complete microscopic resection and patients with stage III and IV thymomas, would be referred to Rigshospitalet, Denmark for further oncological treatment and follow-up.
Chest tube removal
All patients had chest tube removal according to guideline for our department. No air leakage and production of less than 400 mL of pleural fluid in the chest tube over a period of 24 hours after surgery or less than 100 mL during the first 6 hours after surgery.
Results
Surgical complications
There were no conversions of the surgical approach in each of the minimal invasive groups.
Only a few patients experienced complications to surgery in all groups (Table 1). Therefore, no statistical analysis has been made on these data. Totally, seven patients had postoperative pneumothorax (Table 1), whereas 2 of the patients did not require chest tube treatment. Both patients were in the RATS group.

Full table
No patients in the RATS group died within 30 days postoperatively. One patient in the VATS group was readmitted 9 days postoperatively at a local hospital with a hypovolemic shock with hemothorax caused by fall episode at home resulting in death of the patient, but not related to the surgery.
Among the patients that were treated with open surgery, a single patient had chylothorax and one patient died during admission due to sepsis from pneumonia.
Peri- and postoperative results
There was no significant difference in median age between the groups but there were significantly more female patients in the open surgery group compared with the minimal invasive groups (Table 2). We found that the RATS patients had a significantly higher Masaoka-Koga stage compared to the VATS and sternotomy groups, while no difference was found between VATS and sternotomy (Table 3). Patients operated with minimal invasive approach (RATS and VATS) were admitted significantly shorter time than patients, who underwent open surgery. However, there was no statistically significant difference in the length of hospital stay between patients operated with VATS and RATS technique (Table 4).
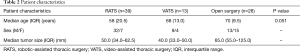
Full table
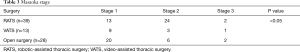
Full table
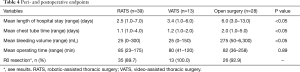
Full table
Patients operated with minimal invasive approach (RATS and VATS) had a significantly shorter time with a chest tube than patients operated with open approach but there was no significant difference between RATS and VATS technique.
Patients undergoing RATS and VATS surgery, experienced a significantly lower blood loss compared to patients undergoing open surgery (Table 4). No significant difference in blood loss volume was demonstrated in patients treated with RATS and VATS technique. There was no significant difference in mean operating times between the three groups.
R0 resection and stadium III patients
Radical resection by the pathology report was not obtained for four RATS patients and two patients in the open surgery group (Table 4). The four patients in the RATS group were all in stage II. The site for incomplete resection were in three cases discontinuous thymoma capsule caused by electro-cauterization while the fourth patient was re-resected with open surgery afterwards without malignant finding. None of the four patients have had recurrence during 4, 5, 5 and 6 years follow-up respectively. Among stage III patients, two patients with open surgery had invasion of the brachiocephalic vein and mediastinal pleura and did not achieve radical surgery at the site of the mediastinal pleura which was treated at Rigshospitalet, Denmark with radiation therapy with no recurrence for nine years in one patient while the other died the year after surgery. In the RATS group one patient had invasion of the pericardium and had radical surgery while two patients operated respectively by VATS and RATS, we found invasion of the mediastinal pleura and both had radical surgery.
Discussion
Robotic assisted resection of an anterior mediastinal mass was introduced for the first time in 2001 by Yoshino et al. (12). However, only a low number of studies have published their experience with RATS thymectomy. In this retrospective study, we have analyzed our results during a 11-year period comparing three different surgical approaches RATS, VATS and open surgery in the surgical treatment of thymomas respectively.
In our study, minimal invasive surgery in terms of “RATS” and “VATS” have shown their superiority in terms of admission time, chest tube time and blood loss throughout the surgery compared to open surgery. However, there was no significant difference between RATS and VATS, when it comes to length of hospital stay, chest tube time and surgical blood loss. These results are consistent with a recent publication demonstrating less blood loss and shorter admission time after RATS compared to open surgery (9,10). However, it must be considered that larger and more complex tumors will more frequently be operated through open surgery while simple thymectomies will be performed through minimal invasive surgery. In opposition to this statement our study demonstrated that patients operated with the RATS technique had more advanced stages than the two other groups but without any impact on length of stay and length of chest tube duration compared to patients operated with VATS. These findings support that the RATS technique could replace open surgery for patients with even advanced tumors in thoracic centers with experience in the RATS technique. However, this is based on a small study with a low number of patients and furthermore a retrospective study with heterogenic baseline characteristics of the patients but underline the necessity to perform a randomized controlled trial comparing open surgery with RATS for patients with an advanced stage thymoma.
In our study we did not find significant difference in the operating time between the three different techniques unlike a previous study demonstrating an increased operating time for patients operated with the RATS technique compared to open surgery (9).
Previously, there has been concerns regarding the risk of incomplete resection of thymomas through VATS (13) but these findings are not consistent with a recent retrospective study, where complete R0 resection was achieved for all patients having RATS (10). In our study, four patients in the RATS group had a pathology report where the capsule was destroyed in small areas due to spreading of heat from the permanent cautery spatula. One patient in the RATS group did undergo re-resection through sternotomy, without finding further malignancy.
In all patients the border between the pericardium and the specimen was clearly free and without invasion macroscopically but these patients were recorded with discontinuous thymoma capsule in small areas and following, complete radicality could not be warranted by the pathologist. We believe that these patients had radical surgery microscopically too which is consistent with the finding that none of the patients have had recurrences in their follow-up program and the fourth patient we reoperated with the same finding did not have any malignant tissue left.
The resection border between the pericardium and the thymus is limited to less than 1 mm and therefore spreading of heat was not possible to eliminate from the permanent cautery spatula but the instrument has now been changed to a different electrocautery device with less spreading of heat which solved the problem for the pathologist.
In the VATS group, all patients were radically resected, while two patients in the open surgery group had incomplete resection. Our population size was not large enough to draw any conclusions regarding the safety in terms of complete resection between the three surgical approaches but underline that the RATS technique and possibly open approach were used in more advanced stages and for larger thymomas. In a previous publication it was recommended that thymomas of a size less than 5 cm should be operated through minimal invasive surgery to avoid capsule injury of thymomas (13) and following avoiding a pathology report questioning the radicality. Furthermore, it is worth mentioning that none of the six patients, four RATS and two sternotomy patients respectively did not have any relapse during the follow-up period. A single patient without radical resection in the sternotomy group died within 1 year after surgery.
In this study, the oncological relapse perspective was not included due to a short follow-up period. It has been suggested, that a follow-up period of at least 10 years is required to draw any conclusion regarding relapse rates (13).
The groups in this retrospective study are close to homogenous in terms of choice for the surgical approach and postoperative treatment. The treatment after surgery is without great differences as all patients have been treated in the same department with the same procedures for medication, chest tube removal, discharge from the hospital and follow-up.
Strengths
This is one of the largest single center studies with consecutive inclusion of all patients treated for thymoma with three different techniques, RATS, VATS and open surgery respectively. All patients were treated with a standardized postoperative regimen leading to consistence for the comparison of the outcome.
Limitations
Our study was not a randomized trial but was a single center study with a consecutive inclusion of the patients in a limited number. However, it is difficult to include a higher number of patients due to low incidence of thymomas.
This study is a retrospective study with an inclusion period from 2006 to 2019. Therefore, our follow-up period was too short to draw any conclusion on the incidence of relapse of thymomas.
Conclusions
Minimal invasive surgery seems to be a safe surgical method in the treatment of thymomas. RATS and VATS were associated with a lower blood loss through surgery, shorter admission time and shorter chest tube time compared to open resection. RATS surgery might be considered for patients with a more advanced thymoma stage. However, the oncological perspective has not been investigated in this study. Larger international multicenter randomized controlled trials with a long follow-up are required to draw any conclusions regarding the oncological point of view.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the Transparent Reporting of Evaluations with Nonrandomized Designs (TREND) reporting checklist (available at http://dx.doi.org/10.21037/med-20-56).
Data Sharing Statement: Available at http://dx.doi.org/10.21037/med-20-56
Peer Review File: Available at http://dx.doi.org/10.21037/med-20-56
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/med-20-56). The study has been initiated solely by the authors. The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional board of Odense University Hospital, Denmark with case number 17/44005 as a retrospective quality control study without need for informed consent from the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Duwe BV, Sterman DH, Musani AI. Tumors of the mediastinum. Chest 2005;128:2893-909. [Crossref] [PubMed]
- Srirajaskanthan R, Toubanakis C, Dusmet M, et al. A review of thymic tumours. Lung Cancer 2008;60:4-13. [Crossref] [PubMed]
- Masaoka A, Monden Y, Nakahara K, et al. Follow-up study of thymomas with special reference to their clinical stages. Cancer 1981;48:2485-92. [Crossref] [PubMed]
- Okumura M, Ohta M, Tateyama H, et al. The World Health Organization histologic classification system reflects the oncologic behavior of thymoma: a clinical study of 273 patients. Cancer 2002;94:624-32. [Crossref] [PubMed]
- Ruffini E, Fang W, Guerrera F, et al. The International Association for the Study of Lung Cancer Thymic Tumors Staging Project: The Impact of the Eighth Edition of the Union for International Cancer Control and American Joint Committee on Cancer TNM Stage Classification of Thymic Tumors. J Thorac Oncol 2020;15:436-47.
- Scorsetti M, Leo F, Trama A, et al. Thymoma and thymic carcinomas. Crit Rev Oncol Hematol 2016;99:332-50. [Crossref] [PubMed]
- Fang W, Chen W, Chen G, et al. Surgical management of thymic epithelial tumors: a retrospective review of 204 cases. Ann Thorac Surg 2005;80:2002-7. [Crossref] [PubMed]
- Detterbeck FC, Moran C, Huang J, et al. Which way is up? Policies and procedures for surgeons and pathologists regarding resection specimens of thymic malignancy. J Thorac Oncol 2011;6:S1730-8. [Crossref] [PubMed]
- Marulli G, Comacchio GM, Schiavon M, et al. Comparing robotic and trans-sternal thymectomy for early-stage thymoma: a propensity score-matching study. Eur J Cardiothorac Surg 2018;54:579-84. [Crossref] [PubMed]
- Casiraghi M, Galetta D, Borri A, et al. Robotic-assisted thymectomy for early-stage thymoma: a propensity-score matched analysis. J Robot Surg 2018;12:719-24. [Crossref] [PubMed]
- Detterbeck FC, Stratton K, Giroux D, et al. The IASLC/ITMIG Thymic Epithelial Tumors Staging Project: proposal for an evidence-based stage classification system for the forthcoming (8th) edition of the TNM classification of malignant tumors. J Thorac Oncol 2014;9:S65-S72. [Crossref] [PubMed]
- Yoshino I, Hashizume M, Shimada M, et al. Thoracoscopic thymomectomy with the da Vinci computer-enhanced surgical system. J Thorac Cardiovasc Surg 2001;122:783-5. [Crossref] [PubMed]
- Kimura T, Inoue M, Kadota Y, et al. The oncological feasibility and limitations of video-assisted thoracoscopic thymectomy for early-stage thymomas. Eur J Cardiothorac Surg 2013;44:e214-8. [Crossref] [PubMed]
Cite this article as: El-Akkawi AI, Eckardt J. Comparison of surgical outcomes after robotic assisted thoracic surgery, video-assisted thoracic surgery and open resection of thymoma. Mediastinum 2021;5:11.


