
Cost-effectiveness of endoscopic mediastinal staging
Introduction
Lung cancer is the first cause of cancer-related mortality, with more than two million new cases per year diagnosed worldwide (1). Mediastinal staging has a major role in the definition of the therapeutic strategy in early-stage and locally-advanced non-small cell lung cancer (NSCLC), since upfront surgery is the mainstay of treatment in stages I and II, and induction or definitive chemo- and radio-chemotherapy are indicated in the treatment of stage III tumors. The assessment of nodal status also has a primary role in in the selection of stage I non-surgical candidates for alternative treatments as stereotactic radiotherapy (SBRT) (2). Non-invasive mediastinal staging with CT or PET scans has relatively limited accuracy, with a pooled specificity of 81% and 55% and a sensitivity of 88% and 80%, respectively (3). The association of CT and PET may improve the accuracy of non-invasive staging, but the results remain relatively inaccurate and influenced by factors as histology, size, location and metabolism of the tumor (4,5). Tissue confirmation may therefore be required to reach an adequate definition of nodal status.
Current guidelines recommend invasive staging in patients with clinical N1 to N3 disease, centrally-located or larger than 3 cm tumors (6). However, the ideal invasive mediastinal staging strategy is still a matter for debate, particularly considering the cost-effectiveness of the different approaches. Mediastinoscopy has been for a long time considered the gold standard technique for mediastinal staging of lung cancer. The introduction of videomediastinoscopy has improved the safety and accuracy of the procedure, allowing a more extensive mediastinal nodal sampling and dissection. Lymph-nodes of the upper and lower paratracheal and subcarinal stations can be reached. However, mediastinoscopy has to be performed in the operating theatre under general anesthesia, and does not allow to reach lower mediastinal, sub-aortic and para-aortic nodal stations. Other surgical techniques as video-assisted mediastinal lymphoadenectomy (VAMLA) and transcervical extended mediastinal lymphoadenectomy (TEMLA) may enhance the sensitivity of mediastinal staging by increasing the number of lymph-nodes that can be biopsied or removed, but are more invasive and associated with an increased morbidity, an issue that has limited a widespread diffusion of these procedures (7). Extended mediastinoscopy, introduced in clinical practice by Ginsberg, allows to reach sub-aortic and para-aortic nodes by proceeding with the instrument between the supra-aortic vessels, but has also not gained general acceptance due to the potentially higher risks of the procedure and the relatively lower prognostic role of these nodal stations (8).
In the last two decades, thanks to the technological advancement, endoscopic techniques have gained growing success in the field of mediastinal staging. Factors in favor of the endoscopic approach are a reduced invasiveness in comparison with surgical techniques, a lower procedure-related complication rate and a thorough assessment of mediastinal stations. With the development of instrumentation with convex probes, endobronchial ultrasound with transbronchial biopsy (EBUS-TBNA) and endoscopic ultra-sonography with fine–needle aspiration (EUS-FNA) have been increasingly used. EBUS-TBNA allows to examine not only the paratracheal and subcarinal stations, but also N1 hilar and interlobar nodes (stations 10 and 11). Transesophageal mediastinal staging (EUS-FNA) has a complementary role to EBUS-TBNA, giving access to stations 5, 8 and 9. Some Authors have therefore suggested a combined ultrasound (CUS) approach, with endoscopic techniques as the mainstay of mediastinal staging (9).
However, the cost-effectiveness of the different invasive and non-invasive approaches is still a matter for debate, and several issues concerning mediastinal staging still have to be assessed. One of the main points concerns the diagnostic accuracy and cost-effectiveness of the different methods according to nodal metastases prevalence. Moreover, complication-rate, costs, impact of the procedures on quality of life, survival and time required to complete the staging process before starting treatment still have to be analyzed in detail. The ideal combination of different staging techniques to improve the cost-effectiveness of mediastinal staging is also a matter for discussion.
Factors influencing the accuracy and cost-effectiveness of surgical and endoscopic techniques
According to the current European Society of Thoracic surgeons (ESTS) guidelines for invasive mediastinal staging of lung cancer, cytological or histological samples of at least the subcarinal and right and left lower paratracheal lymph nodes (stations 7, 4R and 4L) must be obtained. Moreover, the right and left upper paratracheal nodes (2R and 2L) should also be biopsied if visible (6). Mediastinoscopy has been until recently considered the gold standard technique for invasive mediastinal staging, and a benchmark for the comparison of the results of new techniques. In a study performed by Yasufuku et al. in a cohort of 153 patients with early-stage lung cancer, the sensitivity, diagnostic accuracy and NPV of mediastinoscopy were 79%, 90% and 93% (10). An important point to be analyzed is the influence of nodal prevalence on the diagnostic accuracy and cost-effectiveness of mediastinoscopy, an issue that also concerns the other staging methods. In a study performed from 1999 to 2004, Meyers et al. observed that systematic standard mediastinoscopy was not cost-effective in a group of patients with clinical stage I NSCLC and a N2 occult disease prevalence of 5.6%. In fact, the estimated increase in survival was only 0.008 years, with a cost per gained life year of 250.989 $. Conversely, systematic mediastinoscopy was cost-effective when the prevalence of nodal disease was higher than 10%, with a reduction of the costs per gained life year to 100.000 $. However, the sensitivity of mediastinoscopy in this study was only 38% (11). The introduction of video-assisted mediastinoscopy may have increased the sensitivity and cost-effectiveness of the technique. In fact, according to a more recent meta-analysis the pooled sensitivity of video-mediastinoscopy was 89%, and was less dependent on nodal metastases prevalence (3). Other factors as 18-FDG tumor uptake during PET scan may also influence the results of staging. Fernandez et al. observed that systematic mediastinoscopy was not cost-effective in patients with T1–2 N0 tumors and a SUV max higher than 10, since only 1 out of 90 patients had occult nodal metastases (12). The results of metabolic assessment may also influence the results of endoscopic staging, since Chouaid et al. observed that the sensitivity and NPV of EBUS-TBNA were respectively 90.4% and 75.7% in patients with a positive PET scan and 83.3% and 96.6% in patients with negative PET scans (13). Other studies show that the accuracy of EBUS-TBNA is influenced by the use of preliminary non-invasive staging. In fact, Gu et al. observed in a meta-analysis including 1,299 patients that the pooled sensitivity was 94% in presence of pathological CT or PET imaging, and 76% when the patients were not selected according to CT and PET findings (14).
The diagnostic yield of surgical and endoscopic staging techniques has been compared in several studies. Ge et al. performed a meta-analysis to compare the sensitivity of EBUS-TBNA and videomediastinoscopy, and observed a pooled sensitivity of 84% and 86%, respectively (15). Other studies also reported better results with EBUS-TBNA than with mediastinoscopy. Um et al. analyzed a cohort of patients with cN1–N3 NSCLC and a 59.1% prevalence of mediastinal nodal disease to compare the results of mediastinoscopy and EBUS-TBNA. The sensitivity and NPV of EBUS and mediastinoscopy were 88% and 85% and 81% and 79%, respectively. The authors therefore suggested using endoscopy as the first step for invasive mediastinal staging of lung cancer (16).
However, factors as operator expertise with EBUS-TBNA may influence the cost-effectiveness of the procedure. In fact, Kheir et al. observed that competence with the technique was reached only after 55 to 60 procedures, with an increase of the diagnostic accuracy from 72% to 88% (17). Another factor that may influence the accuracy of endoscopic mediastinal staging is the extent of nodal sampling. During systematic EBUS, stations 4R, 4L and 7 should be sampled if larger than 5 mm, as any lymph node larger than 1 cm at CT scan or FDG-avid (SUV >2.5). Conversely, during systematic EUS stations 4L, 7, 8 and any pathological nodes at CT or PET should be biopsied (6,18). However, in a multicenter study performed by Bousema et al., a significant number of examinations were not in accordance with the guidelines, since in 30% of the procedure biopsies were performed only on pathological nodes at CT or PET imaging (19). This issue is underscored by Sanz-Santos et al., who observed in a retrospective study that systematic nodal biopsy during EBUS-TBNA was associated with an increased accuracy of the staging by 13% in comparison with a targeted endoscopic approach based only on CT and PET features (20).
Other potentially limiting factors for endoscopic staging concern the presence of micrometastases, which are under the diagnostic threshold of EBUS-TBNA, or a partial involvement of the lymph-nodes of the nodal stations. Moreover, due to anatomical factors stations 5 and 6 cannot be assessed with EBUS-TBNA, even if a trans-pulmonary artery biopsy technique has been described (21). EUS-FNA has been proposed as a viable strategy to overcome these limitations. A potential advantage of the technique is the possibility of assessing nodes outside the reach of EBUS-TBNA, as those of stations 5, 8 and 9. Micames et al. performed a meta-analysis to evaluate the results of EUS-FNA in mediastinal lung cancer staging, and observed a 90% sensitivity in patients with pathological nodes at CT or PET, reduced to 58% in patients with a normal non-invasive mediastinal assessment (22).
These results demonstrate that despite the continuous development of staging techniques, no single procedure reaches optimal results in terms of diagnostic accuracy and cost-effectiveness. A strategy to be analyzed concerns therefore the association of surgical and endoscopic techniques.
Influence of a combined staging approach on cost-effectiveness
The association of endoscopic and surgical staging procedures as EBUS-TBNA, EUS and videomediastinoscopy could potentially improve the cost-effectiveness of mediastinal staging. Some Authors have in particular proposed a combined endoscopic approach with EBUS and EUS (CUS). This approach could theoretically enhance the number of accessible nodal stations, therefore potentially increasing the sensitivity and NPV. Szlubowski et al. reported a sensitivity, specificity, diagnostic accuracy, PPV and NPV with CUS of 68%, 98%, 91%, 91% and 91%, respectively (9). Hwangbo et al. also observed that the association of EUS to EBUS increased the sensitivity and NPV of nodal staging in operable NSCLC respectively from 84% and 93% to 91% and 96% (23). Accordingly, Crombag et al. observed that adding EUS to EBUS improved the sensitivity of nodal staging by 9% (24). The potential limits of the approach are an increase of costs due to a longer duration of the procedure and the need of different instruments, although the use of the same endoscope to perform both procedures could be a viable option (EUS-B-FNA) (25). Due to these factors and since expertise with both techniques is required, CUS has not gained widespread acceptance yet, and at present EBUS is considered the first step for endoscopic staging, followed by EUS when nodal stations are not in the reach of EBUS. According to the European Society of Gastrointestinal Endoscopy (ESGE), endosonographic assessment with EBUS-TBNA, and when available with EUS-FNA, should be considered the first step during invasive mediastinal staging, followed by surgical staging in case of negative results (18). Kang et al. observed that the use of either technique as the first procedure did not alter the accuracy of mediastinal staging, and therefore advised using EBUS-TBNA as the initial method (26).
Another issue to consider is the optimal combination of surgical and endoscopic staging to improve the diagnostic accuracy, considering that confirmatory mediastinoscopy after negative EBUS-TBNA may find unforeseen metastases in about 8% of the patients (19). The ASTER (Assessment of Surgical Staging vs. Endosonographic Ultrasound in Lung Cancer: a Randomized Clinical Trial) multicenter randomized trial recruited 241 patients with resectable lung cancer and a 55% nodal metastases prevalence to compare the results of surgical staging alone with endoscopic staging and confirmatory mediastinoscopy after negative ultrasound assessment. Sensitivity was 79% in the surgical study arm, and 85% in the group submitted to endoscopic staging, which was increased to 94% after confirmatory mediastinoscopy. The negative predictive value was 79% in the surgical staging group and 93% in the endoscopic-surgical study arm. Another important result of the study was the reduction of unnecessary thoracotomies from 18% to 7% with the combined approach (27).
In another study, Yasufuku et al. observed that mediastinoscopy and EBUS-TBNA had equivalent sensitivity and NPV in a cohort of patients with 35% nodal metastases prevalence. Since the use of mediastinoscopy after EBUS was associated to an increase of the negative predictive value of only 5%, these Authors considered that a systematical use of mediastinoscopy after negative EBUS-TBNA was not cost-effective in a cohort of patients with a low prevalence of nodal metastases (10). However, the role of confirmatory mediastinoscopy may still be relevant in subgroups of patients with a higher prevalence of nodal metastases. Therefore, despite the pivotal role of endoscopy in mediastinal staging, surgical procedures are still required to reduce the number of false negative-results of EBUS and EUS. The American College of Chest Physicians (ACCP), European Society of Thoracic Surgeons (ESTS) and European Society for Medical Oncology (ESMO) mediastinal staging guidelines thus state that patients with resectable lung cancer at high risk of mediastinal involvement should be staged with EBUS-TBNA or EUS, with videomediastinoscopy to be added in case of negative endoscopic staging (3,6,28).
Tumors with a high risk of mediastinal involvement include those with N1 disease. Decaluwé et al. reported a sensitivity and NPV of 73% and 92% of videomediastinoscopy or VAMLA in a group of 105 patients with cN1 NSCLC and a 26% prevalence of mediastinal nodal involvement (29). In another multicenter prospective study recruiting 100 patients with resectable cN1 NSCLC and a N2 prevalence of 24%, Dooms et al. compared EBUS or CUS with a combined endosonography and confirmatory mediastinoscopy approach. They observed that the sensitivity and NPV in the two groups were 38% and 81%, and 73% and 91%, respectively, demonstrating that a combined surgical and endoscopic mediastinal staging approach also has a role in cN1 tumors (30).
Procedure-related morbidity
In a meta-analysis performed by Bousema et al., the overall complication rate of mediastinoscopy was 6.0%, with a mortality of 0.5%. Major morbidity (Clavien-Dindo grade III or IV) was observed in 1.9% of the patients. Potential complications of mediastinoscopy include haemorrhage, which may be fatal due to the lesion of major vessels, cervical or mediastinal infections, pneumothorax and esophageal lesions. One of the most frequently observed complications is recurrent laryngeal palsy, reported in 2.8% of the patients (31). The incidence of procedure-related morbidity is increased in case of re-do mediastinoscopy and after chemotherapy or radiotherapy. The complication rate of EBUS-TBNA compares favourably with that of mediastinoscopy. In a retrospective multicenter trial, Von Bartheld et al. analyzed 14,075 EUS-FNA and 2,675 EBUS procedures, and observed a 0.04% mortality rate, mainly related to the poor performance status of the patients (American Society of Anesthesiologists score of III/IV). In this series, serious adverse events had an incidence of 0.15% (0.16% after EUS and 0.11% after EBUS). They were more often of infectious origin, particularly mediastinal, although haemorrhage, pneumomediastinum and sedation related complications were also present (32).
In the multicenter randomized ASTER trial, the incidence of complications in the surgical and combined endoscopic (EBUS-TBNA and EUS-FNA) and surgical approach was respectively 6% and 5%. However, the only observed complication after endosonography was a pneumothorax; on the contrary twelve complications were observed after surgery, the most frequent being recurrent laryngeal nerve palsy (27). In a meta-analysis performed by Ge et al. seventeen complications were observed in 915 patients after mediastinoscopy, and four minor complications in 999 patients who underwent EBUS-TBNA. No mortality was observed in any of the groups (15). These results demonstrate the lower incidence of complications associated with endoscopic staging, showing that a reduction of the number of surgical procedures could improve the cost-effectiveness of staging in terms of complication-rate.
Costs of the different staging approaches
One of the main issues concerning the cost-effectiveness of the staging approaches are the costs for the healthcare system, which have to be balanced against the benefits of the procedure in terms of quality of life, gained life years and impact of the staging process on the time delay to treatment and long-term survival. Steinfort et al. observed that EBUS-TBNA with surgical confirmation of negative results was the least expensive staging approach, provided the sensitivity of EBUS-TBNA was at least 20%. In particular, initial staging with EBUS-TBNA was more cost-effective than conventional TBNA and mediastinoscopy. Moreover, when the degree of nodal involvement was taken into account, surgical confirmation after EBUS-TBNA became cost-effective when the prevalence of lymph node metastases was higher than 79%, confirming the influence of nodal metastases prevalence on the cost-effectiveness of the staging approaches (33). In another decision tree model analysis Harewood et al. observed that EUS-FNA remained the least costly strategy as long as the probability of lymph node metastases was lower than 32%. With a higher nodal involvement prevalence, the combination EUS-FNA/EBUS-TBNA was the preferred option (34).
The introduction of new endoscopic staging techniques may reduce the costs of staging. Callister et al. calculated the expected saving of the use of EBUS-TBNA in lieu of conventional TBNA and mediastinoscopy. In a group of 47 non-small cell lung cancer patients, of which 25 expected to be true positive at mediastinal staging by EBUS-TBNA, they calculated the possibility for the local healthcare system to save with this strategy £32,631 per year (about £1,300 for each patient) (35). However, a point to consider is the availability of ultrasound endoscopes. With the advent of EBUS-TBNA, the role of conventional TBNA has declined due to its lower sensitivity and NPV, despite the reduced costs. However, EBUS and EUS may not be available in several centers around the world, especially in low-income countries. Lack of expertise in low-volume centers may also significantly reduce the diagnostic yield of EBUS-TBNA. Surgical staging with mediastinoscopy may still therefore be the procedure of choice for mediastinal staging in a relevant number of thoracic surgery units. Moreover, older but cheaper minimally-invasive techniques as conventional TBNA without ultrasound guidance may still have a specific role in mediastinal staging. With the aim of reducing the costs of staging, Liran et al. proposed a combined approach with TBNA and EBUS-TBNA, tailored according to the site of nodal stations and lymph-node size. In their study, conventional TBNA had an acceptable diagnostic yield when used to biopsy lymph-nodes ≥20 mm of nodal stations 7, 4R and 11R. However, considering its lower sensitivity, the role of TBNA seems at present useful only when more ultrasound endoscopy is not available or not sustainable (36). In fact, Wallace et al compared (EBUS/EUS), EBUS alone, EUS alone, and TBNA and observed a sensitivity of 93%, 69%, 69%, and 35%, respectively (37).
Impact of mediastinal staging on quality of life, costs and treatment
The impact of mediastinal staging on survival and quality of life remains a main issue in the definition of the optimal strategy. Czarnecka-Kujawa et al. recently performed a study with a decision tree model analysis to assess within the Canadian healthcare system the cost-effectiveness of different mediastinal staging strategies in patients with clinical T1N0 peripheral lung tumors, measuring Quality-adjusted life years (QALY) and incremental cost effectiveness ratios (ICER). Invasive staging with EBUS-TBNA followed by confirmatory mediastinoscopy was associated with a better outcome in terms of QALYs if compared with EBUS-TBNA or mediastinoscopy (respectively 5.88, 5.87 and 5.86 QUALYs), despite being the most expensive strategy. However, the cost-effectiveness of the different procedures varied according to the prevalence of nodal metastases. In fact, when the nodal disease prevalence was between 2.5% and 57%, an EBUS-TBNA based strategy was the most cost-effective (~$80,000/QUALY). On the other hand, an EBUS-TBNA and confirmatory mediastinoscopy approach was more cost-effective when nodal metastases prevalence was higher than 57% (~$79,000/QUALY). Another important point to consider is that these results were observed when the endoscopic procedure was performed under conscious sedation outside the operating theatre (Table 1). The type of anesthesia and setting of the procedures may therefore have a significant impact on the cost-effectiveness. Moreover, costs of the national healthcare systems may vary, influencing the comparison of trials performed in different countries (38).
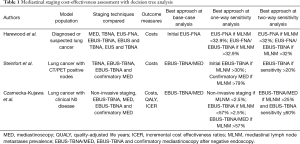
Full table
In fact, in a prospective multicentric French trial recruiting 231 patients with a 52% mean nodal metastases prevalence, Chouaid et al. observed that EBUS-TBNA was more cost-effective than systematic mediastinoscopy as the initial staging procedure, with a saving of €1,450 per patient. Notably, 75% of the endoscopic procedures were performed under general anesthesia, a point in contrast with the results of the study by Czarnecka-Kujawa et al. In fact, the Authors calculated that if all the procedures had been carried out under general anesthesia, an expected saving of €994 per patient would still have been observed. Conversely, no advantage would have been present if the costs of EBUS had been higher than €1,834 (13). In another study, Andrade et al. compared the direct and indirect costs of mediastinoscopy and EBUS-TBNA. The procedures were performed in the OR and direct hospital costs and indirect costs related to hospital waste production were evaluated. The results of the study show that the direct costs were $2,356 for mediastinoscopy and $2,503 for EBUS-TBNA, but the amount of solid waste, and therefore the costs, were higher with mediastinoscopy (1.8 vs. 0.5 kg) (39).
The number of unnecessary surgical procedures avoided thanks to invasive staging is also of primary importance, considering both costs and quality of life. Sharples et al. observed in the ASTER trial that endosonography, followed by confirmatory surgical staging, was associated with a lower number of unnecessary thoracotomies in comparison with surgical staging. Accordingly, the 6-month costs were £9,713 per patient in the endosonography-based strategy and £10,459 in the surgical group. The approach including ultrasonography was also associated with a better quality of life, measured with the European Quality of Life-5 Dimensions (EQ-5D) questionnaire during staging, and was slightly more effective (difference in QALY 0.015). The Authors therefore concluded that the combined endosonography-surgical strategy was the cheapest and most effective approach (40).
In a pragmatic, multicentre randomized controlled study Navani et al. compared a conventional non-endoscopic staging with an EBUS-TBNA or EUS based approach in patients with stage I to IIIA lung cancer, and observed that the endoscopic strategy significantly reduced the time required to reach a therapeutic decision. In fact, an EBUS-TBNA based strategy was associated with a mean delay in treatment of 15 days, significantly shorter than the mean time delay of 30 days observed with the use of standard staging procedures. Moreover, patients in the EBUS group had a lower incidence of unnecessary thoracotomies at 1 year and a better postoperative survival (Table 2). This at an equivalent cost per patient: £2,407 in the EBUS group and £2,348 in the group submitted to conventional diagnostic and staging approach (41).

Full table
Future-issues: extending invasive staging to N1 stations
Preoperative lymph-node staging is at present focused on the definition of mediastinal involvement. However, in the light of a potential evolution of oncological and surgical therapeutic strategies, pre-treatment definition of the N1 status could also be of primary interest. In fact, due to the development of induction protocols for the treatment of stage II disease, pre-treatment assessment not only of mediastinal nodal stations but also of N1 stations could become mandatory. Ongoing trials are also evaluating the role of induction immunotherapy in stage I–IIIa NSCLC, and accurate preoperative N1 staging could also have a primary role in this setting (42). Another main issue concerns the role of segmental resections, which could become in the near future the procedures of choice for the surgical treatment of stage I NSCLC (43). Current strategies to select patients for anatomical segmental resections include intraoperative frozen section analysis and conversion to lobectomy in case of nodal involvement, but a preoperative assessment of N1 stations could allow a better pre- and intraoperative treatment planning, reducing costs and duration of the procedures. Presently available endoscopic instrumentation allows to reach stations 10 and 11 and selected station 12 nodes, but future technological development may allow to approach more peripheral nodal stations by using smaller ultrasound endoscopes (44).
Conclusions
According to the current therapeutic strategy, invasive mediastinal staging has a major role in the treatment of patients with stage I to III NSCLC. Present guidelines advise tissue confirmation in case of CT or PET scan positive mediastinal lymph nodes, clinical N1 disease, tumors larger than 3 cm or centrally-located lesions. EBUS-TBNA and EUS-FNA have a pivotal role in mediastinal staging of NSCLC, with videomediastinoscopy still used to rule out false negative results after negative endoscopic assessment in patients at high risk of mediastinal nodal involvement. However, a standardization of endoscopic and surgical staging according to international guidelines with systematic nodal sampling is essential to maintain adequate results of mediastinal staging. Moreover, specific issues may influence the cost-effectiveness of invasive staging, as the prevalence of mediastinal metastatic involvement, competence with endoscopic techniques and procedure related costs, which may vary in different national healthcare systems. Technological development could allow to overcome the present limits of minimally-invasive nodal staging, an important issue in the light of the evolution of new therapeutic strategies as those including induction treatments in early-stage tumors and parenchyma-sparing anatomic surgical procedures.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Mediastinum for the series “Minimally Invasive (Endoscopic) Mediastinal Staging of Lung Cancer”. The article has undergone external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/med-20-27). The series “Minimally Invasive (Endoscopic) Mediastinal Staging of Lung Cancer” was commissioned by the editorial office without any funding or sponsorship. AC served as the unpaid Guest Editor of the series and an unpaid editorial board member of Mediastinum from Jan 2020 to Dec 2021. The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018;68:394-424. [Crossref] [PubMed]
- Vial MR, Khan KA, O'Connell O, et al. Endobronchial Ultrasound-Guided Transbronchial Needle Aspiration in the Nodal Staging of Stereotactic Ablative Body Radiotherapy Patients. Ann Thorac Surg 2017;103:1600-5. [Crossref] [PubMed]
- Silvestri GA, Gonzalez AV, Jantz MA, et al. Methods for staging non-small cell lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013;143:e211S-50S.
- Wang J, Welch K, Wang L, et al. Negative predictive value of positron emission tomography and computed tomography for stage T1-2N0 non-small-cell lung cancer: a meta-analysis. Clin Lung Cancer 2012;13:81-9. [Crossref] [PubMed]
- Lee PC, Port JL, Korst RJ, et al. Risk factors for occult mediastinal metastases in clinical stage I non-small cell lung cancer. Ann Thorac Surg 2007;84:177-81. [Crossref] [PubMed]
- De Leyn P, Dooms C, Kuzdzal J, et al. Revised ESTS guidelines for preoperative mediastinal lymph node staging for non-small-cell lung cancer. Eur J Cardiothorac Surg 2014;45:787-98. [Crossref] [PubMed]
- Kużdżał J, Warmus J, Grochowski Z. Optimal mediastinal staging in non-small cell lung cancer: what is the role of TEMLA and VAMLA? Lung Cancer 2014;86:1-4. [Crossref] [PubMed]
- Ginsberg RJ, Rice TW, Goldberg M, et al. Extended cervical mediastinoscopy. A single staging procedure for bronchogenic carcinoma of the left lung. J Thorac Cardiovasc Surg 1987;94:673-8. [Crossref] [PubMed]
- Szlubowski A, Zieliński M, Soja J, et al. A combined approach of endobronchial and endoscopic ultrasound-guided needle aspiration in the radiologically normal mediastinum in non-small-cell lung cancer staging–a prospective trial. Eur J Cardiothorac Surg 2010;37:1175-9. [Crossref] [PubMed]
- Yasufuku K, Pierre A, Darling G, et al. A prospective controlled trial of endobronchial ultrasound-guided transbronchial needle aspiration compared with mediastinoscopy for mediastinal lymph node staging of lung cancer. J Thorac Cardiovasc Surg 2011;142:1393-400.e1. [Crossref] [PubMed]
- Meyers BF, Haddad F, Siegel BA, et al. Cost-effectiveness of routine mediastinoscopy in computed tomography- and positron emission tomography-screened patients with stage I lung cancer. J Thorac Cardiovasc Surg 2006;131:822-9. [Crossref] [PubMed]
- Fernandez FG, Kozower BD, Crabtree TD, et al. Utility of mediastinoscopy in clinical stage I lung cancers at risk for occult mediastinal nodal metastases. J Thorac Cardiovasc Surg 2015;149:35-41. [Crossref] [PubMed]
- Chouaid C, Salaün M, Gounant V, et al. Clinical efficacy and cost-effectiveness of endobronchial ultrasound-guided transbronchial needle aspiration for preoperative staging of non-small-cell lung cancer: Results of a French prospective multicenter trial (EVIEPEB). PLoS One 2019;14:e0208992 [Crossref] [PubMed]
- Gu P, Zhao YZ, Jiang LY, et al. Endobronchial ultrasound-guided transbronchial needle aspiration for staging of lung cancer: a systematic review and meta-analysis. Eur J Cancer 2009;45:1389-96. [Crossref] [PubMed]
- Ge X, Guan W, Han F, et al. Comparison of Endobronchial Ultrasound-Guided Fine Needle Aspiration and Video-Assisted Mediastinoscopy for Mediastinal Staging of Lung Cancer. Lung 2015;193:757-66. [Crossref] [PubMed]
- Um SW, Kim HK, Jung SH, et al. Endobronchial ultrasound versus mediastinoscopy for mediastinal nodal staging of non-small-cell lung cancer. J Thorac Oncol 2015;10:331-7. [Crossref] [PubMed]
- Kheir F, Alokla K, Myers L, et al. Endobronchial Ultrasound-Transbronchial Needle Aspiration of Mediastinal and Hilar Lymphadenopathy Learning Curve. Am J Ther 2016;23:e1016-9. [Crossref] [PubMed]
- Vilmann P, Frost Clementsen P, Colella S, et al. Combined endobronchial and esophageal endosonography for the diagnosis and staging of lung cancer: European Society of Gastrointestinal Endoscopy (ESGE) Guideline, in cooperation with the European Respiratory Society (ERS) and the European Society of Thoracic Surgeons (ESTS). Eur J Cardiothorac Surg 2015;48:1-15. [Crossref] [PubMed]
- Bousema JE, van Dorp M, Hoeijmakers F, et al. Guideline adherence of mediastinal staging of non-small cell lung cancer: A multicentre retrospective analysis. Lung Cancer 2019;134:52-8. [Crossref] [PubMed]
- Sanz-Santos J, Serra P, Torky M, et al. Systematic compared with targeted staging with endobronchial ultrasound in patients with lung cancer. Ann Thorac Surg 2018;106:398-403. [Crossref] [PubMed]
- Mehta RM, Biraris PR, Pattabhiraman V, et al. Defining expanded areas in EBUS sampling: EBUS guided trans- and intra-pulmonary artery needle aspiration, with review of transvascular EBUS. Clin Respir J 2018;12:1958-63. [Crossref] [PubMed]
- Micames CG, McCrory DC, Pavey DA, et al. Endoscopic ultrasound-guided fine-needle aspiration for non-small cell lung cancer staging: A systematic review and meta-analysis. Chest 2007;131:539-48. [Crossref] [PubMed]
- Hwangbo B, Lee GK, Lee HS, et al. Transbronchial and transesophageal fine-needle aspiration using an ultrasound bronchoscope in mediastinal staging of potentially operable lung cancer. Chest 2010;138:795-802. [Crossref] [PubMed]
- Crombag LMM, Dooms C, Stigt JA, et al. Systematic and combined endosonographic staging of lung cancer (SCORE study). Eur Respir J 2019;53:1800800 [Crossref] [PubMed]
- Szlubowski A, Zieliński M, Soja J, et al. Accurate and safe mediastinal restaging by combined endobronchial and endoscopic ultrasound-guided needle aspiration performed by single ultrasound bronchoscope. Eur J Cardiothorac Surg 2014;46:262-6. [Crossref] [PubMed]
- Kang HJ, Hwangbo B, Lee GK, et al. EBUS-centred versus EUS-centred mediastinal staging in lung cancer: a randomised controlled trial. Thorax 2014;69:261-8. [Crossref] [PubMed]
- Annema JT, van Meerbeeck JP, Rintoul RC, et al. Mediastinoscopy vs endosonography for mediastinal nodal staging of lung cancer: a randomized trial. JAMA 2010;304:2245-52. [Crossref] [PubMed]
- Postmus PE, Kerr KM, Oudkerk M, et al. Early and locally advanced non-small-cell lung cancer (NSCLC): ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2017;28:iv1-iv21. [Crossref]
- Decaluwé H, Dooms C, D'Journo XB, et al. Mediastinal staging by videomediastinoscopy in clinical N1 non-small cell lung cancer: a prospective multicentre study. Eur Respir J 2017;50:1701493 [Crossref] [PubMed]
- Dooms C, Tournoy KG, Schuurbiers O, et al. Endosonography for mediastinal nodal staging of clinical N1 non-small cell lung cancer: a prospective multicenter study. Chest 2015;147:209-15. [Crossref] [PubMed]
- Bousema JE, van Dorp M, Noyez VJJM, et al. Unforeseen N2 Disease after Negative Endosonography Findings with or without Confirmatory Mediastinoscopy in Resectable Non-Small Cell Lung Cancer: A Systematic Review and Meta-Analysis. J Thorac Oncol 2019;14:979-92. [Crossref] [PubMed]
- von Bartheld MB, Annema JT. Endosonography-related mortality and morbidity for pulmonary indications: a nationwide survey in the Netherlands. Gastrointest Endosc 2015;82:1009-15. [Crossref] [PubMed]
- Steinfort DP, Liew D, Conron M, et al. Cost-benefit of minimally invasive staging of non-small cell lung cancer: a decision tree sensitivity analysis. J Thorac Oncol 2010;5:1564-70. [Crossref] [PubMed]
- Harewood GC, Pascual J, Raimondo M, et al. Economic analysis of combined endoscopic and endobronchial ultrasound in the evaluation of patients with suspected non-small cell lung cancer. Lung Cancer 2010;67:366-71. [Crossref] [PubMed]
- Callister ME, Gill A, Allott W, et al. Endobronchial ultrasound guided transbronchial needle aspiration of mediastinal lymph nodes for lung cancer staging: a projected cost analysis. Thorax 2008;63:384. [Crossref] [PubMed]
- Liran L, Rottem K, Gregorio FZ, et al. A novel, stepwise approach combining conventional and endobronchial ultrasound needle aspiration for mediastinal lymph node sampling. Endosc Ultrasound 2019;8:31-35. [Crossref] [PubMed]
- Wallace MB, Pascual JM, Raimondo M, et al. Minimally invasive endoscopic staging of suspected lung cancer. JAMA 2008;299:540-6. [Crossref] [PubMed]
- Czarnecka-Kujawa K, Rochau U, Siebert U, et al. Cost-effectiveness of mediastinal lymph node staging in non-small cell lung cancer. J Thorac Cardiovasc Surg 2017;153:1567-78. [Crossref] [PubMed]
- Andrade RS, Podgaetz E, Rueth NM, et al. Endobronchial ultrasonography versus mediastinoscopy: a single institution cost analysis and waste comparison. Ann Thorac Surg 2014;98:1003-7. [Crossref] [PubMed]
- Sharples LD, Jackson C, Wheaton E, et al. Clinical effectiveness and cost-effectiveness of endobronchial and endoscopic ultrasound relative to surgical staging in potentially resectable lung cancer: results from the ASTER randomised controlled trial. Health Technol Assess 2012;16:1-75. [Crossref] [PubMed]
- Navani N, Nankivell M, Lawrence DR, et al. Lung cancer diagnosis and staging with endobronchial ultrasound-guided transbronchial needle aspiration compared with conventional approaches: an open-label, pragmatic, randomised controlled trial. Lancet Respir Med 2015;3:282-9. [Crossref] [PubMed]
- Ghysen K, Vansteenkiste J. Immunotherapy in patients with early stage resectable non-small cell lung cancer. Curr Opin Oncol 2019;31:13-7. [Crossref] [PubMed]
- Onaitis MW, Furnary AP, Kosinski AS, et al. Equivalent survival between lobectomy and segmentectomy for clinical stage IA lung cancer. Ann Thorac Surg 2020; [Epub ahead of print]. [Crossref] [PubMed]
- Patel P, Wada H, Hu HP, et al. First Evaluation of the New Thin Convex Probe Endobronchial Ultrasound Scope: A Human Ex Vivo Lung Study. Ann Thorac Surg 2017;103:1158-64. [Crossref] [PubMed]
Cite this article as: Carretta A. Cost-effectiveness of endoscopic mediastinal staging. Mediastinum 2020;4:18.


