Management of bleeding complications during thoracoscopic thymectomy
Introduction
Video-assisted thoracoscopic surgery (VATS) has been increasingly applied in thymectomy as an acceptable approach, although median sternotomy still remains the standard one for surgical resection of thymic tumours (1). During minimally invasive thymectomy, it is crucial to dissociate and expose the thymic veins and the left innominate vein carefully. Intraoperative bleedings are mainly caused by injuries to these veins. And injury of thymic veins or innominate vein need to be managed differently. Thymic veins are usually small in calibre but often vary in number and location. And injury to the thymic veins could be readily controlled when the bleeding site is well identified (2). However, bleeding from the left innominate vein injury is usually difficult to manage thoracoscopically, because of the narrow retro-sternal working space and continuous high blood flow. Since such bleeding complications, which may be catastrophic and often lead to immediate conversion to open surgery, may occur no matter whether the surgeon has completed his learning curve or not (3,4), successful control under VATS is crucial for the safety of the patient and the success of the procedure. We hereby report strategies for safe and effective bleeding control during VATS thymectomy.
Clinical vignette
The first case was an 80-year-old male patient with an incidentally detected right anterior mediastinal mass 18 months ago. The mass enlarged from 3 to 4.6 cm in size. He was diagnosed with cystic thymoma through CT scan and Magnetic resonance imaging (MRI), which showed low signal intensity on T1 images and high signal intensity on T2 images, with moderate enhancement. Injury to a thymic vein below the left innominate vein occurred during a right VATS thymectomy. It was well managed by endovascular clips under VATS. Intraoperative blood loss was 50 mL. The drainage tubes were removed on postoperative day (POD) 2, and the patient was discharged on POD 3 (Table 1). Histopathological examination after surgery confirmed the lesion to be a type AB cystic thymoma with no invasion.
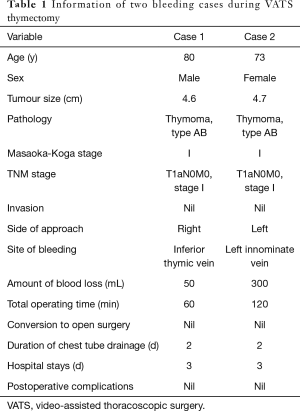
Full table
The second case was a 73-year-old lady who presented to the Shanghai Chest Hospital with an incidentally discovered mediastinal mass. Chest CT scan showed a mass in the left anterior mediastinum measuring 4.7 cm × 2.0 cm. MRI with contrast showed low signal intensity on T1 images and high signal intensity on T2 images with moderate enhancement, suggesting the diagnosis of thymoma. During a left approach VATS thymectomy, massive bleeding from the left innominate vein occurred due to inadvertent injury. But it was successfully controlled via endoscopic stapler. Intraoperative blood loss was 300 mL and the patient did not receive any blood transfusion. Postoperative course was uneventful. Drainage tubes were removed on POD 2, and the patient was discharged on POD 3. The final histopathological examination confirmed the diagnosis of a type AB thymoma.
Operative techniques
We used the conventional three-port technique for VATS thymectomy. The first 10 mm camera and carbon dioxide insufflation port was placed at the level of the 5th intercostal space in the mid-axillary line. The second 10 mm port was placed in the 4th intercostal space in the mid-clavicular line for ultrasonic scalpel, and the third 5 mm port was placed at anterior axillary line in the 3rd intercostal space for grasping the perithymic tissues.
Active and alert mind and always keeping the open thoracic surgery instruments by the side of the operating table
Safety is always the primary concern. It is our routine practice to keep the open thoracic surgery instruments, including the sternum saw, available by the side of the operating table just in case bleeding control under VATS could not be achieved and conversion is considered necessary.
Immediate attention and application of pressure gauze over the bleeding site
When inadvertent injuries occurred during dissection of the thymus, through the 4th intercostal space port, small gauze ribbon was applied immediately with grasping forceps over the vein to stop bleeding.
Identifying the exact site and size of bleeding
Generally, the junction of thymic vein draining to the left innominate vein is the most common site of bleeding, followed by thymic veins (3,4). After clearing the blood accumulated in the working space, the gauze ribbon was removed and with the assistance of the continuous sucking device, the exact bleeding site could be identified.
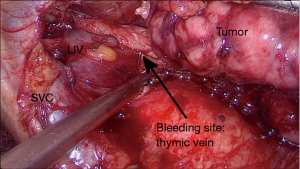
Application of thoracoscopic endoscopic clips in thymic vein injury
In case of bleeding from a thymic vein, endoscopic clips, ultrasonic scalpel, or tissue sealing agents can be used to control the bleeding site (2). We used endoscopic clips thoracoscopically through the mid-clavicular port (Figure 1), when there was enough length of the vein exposed and bleeding was not massive. If the residual thymic vein stump is difficult to be identified or too short for a clip to be applied, it is safer to control the bleeding with endoscopic staplers applied over the left innominate vein as mentioned below.
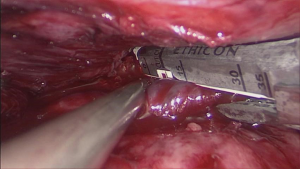
Application of endoscopic staplers in innominate vein injury
After the left innominate vein was exposed using ultrasonic scalpel, a 30 mm endovascular stapler through the mid-clavicular port were applied tangentially over the vein with the help of continuous suction over the bleeding site (Figure 2). After the vein was divided, additional endoclips could be used if there was still minor bleeding from the vessel stumps. This is the safest, quickest, and the most effective way to control massive bleeding from the left innominate vein injury thoracoscopically that occurs during VATS thymectomy (Video 1).
Comments
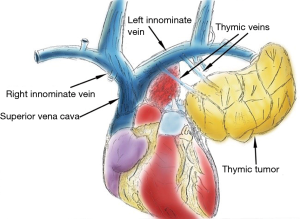
The purpose of this study is how to manage bleeding complications during VATS thymectomy. We reviewed literature focusing on bleeding complications during VATS thymectomy between January 2000 and August 2019. We found that the thymic vein, left innominate vein, internal mammary vessels and superior vena cava (SVC) were the most common vascular structures that could be injured inadvertently (3,5) (Figure 3). Careful interpretation of preoperative CT imaging can provide useful information on the relationship of the thymic tumour with the neighbouring vascular structures and may decrease the risk of bleeding during operation (6,7).
But even with meticulous dissection, these iatrogenic injuries could not be completely avoided. Such bleeding can sometimes be catastrophic which should not only be avoided but also be handled with utmost care. Bleedings from the thymic veins can be safely controlled with ultrasonic scalpel, tissue sealing agents (2,8), or haemostatic vascular clips, as is shown in our first case. Similarly, injury to the internal mammary vessels can usually be dealt with endoclips or tissue sealing agents (8).
If bleeding occurs from the left innominate vein, it is usually more dangerous and difficult to cope with, because of the very limited working space in the retro-sternum in the upper mediastinum and massive bleeding due to continuous high blood flow. It has been reported that SVC injury might be dealt thoracoscopically with either intra-corporeal suturing or limited tangential resection of the segment for haemostasis (3,5). But most often than not it is very demanding and risky to suture the vein under VATS at this place. Immediate and effective measures should be taken to control the bleeding as soon as possible to ensure patients’ safety. It has thus been suggested that innominate vein injuries should be managed via immediate conversion to open sternotomy or thoracotomy and haemostasis be secured with surgical sutures (5,9). Our simple technique of using endoscopic staplers to divide the injured vessel can resolve the problem safely and efficiently, without complex manoeuvres. Dividing the left innominate vein does little harm to the patients, except for some mild complications, such as left upper limb swelling and dizziness, which can be well treated with conservative therapy as collaterals venous drainage develop (10,11).
In conclusion, bleeding during VATS thymectomy from inadvertent thymic vein or innominate vein injury needs to be attended immediately and efficiently. And our experience shows that endoscopic clipping or stapling respectively can provide safe, quick, and effective control of different types of bleedings under VATS. This technique is helpful to ensure the safety and success of minimally invasive surgery for thymic diseases.
Acknowledgments
Funding: This study was supported by Graded treatment of advanced thymoma under the guidance of multi-dimensional histology (YJXT20190104).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/med-20-35). The authors report grants from Graded treatment of advanced thymoma under the guidance of multi-dimensional histology (YJXT20190104), during the conduct of the study. WF serves as an unpaid Editor-in-Chief of Mediastinum. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committees and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Gu Z, Chen C, Wang Y, et al. Video-assisted thoracoscopic surgery versus open surgery for Stage I thymic epithelial tumours: a propensity score-matched study. Eur J Cardiothorac Surg 2018;54:1037-44. [Crossref] [PubMed]
- Wu H, Lin Q, Liu Y, et al. The safety of thymic vein sealing with ultrasonic energy in video-assisted thoracoscopic surgery thymectomy. J Thorac Dis 2019;11:3421-6. [Crossref] [PubMed]
- Villa M, Sarkaria IS. Great Vessel Injury in Thoracic Surgery. Thorac Surg Clin. 2015;25:261-78. [Crossref] [PubMed]
- Yano M, Numanami H, Yamaji M, et al. A pitfall of thoracoscopic thymectomy: a case with intraoperative and postoperative complications. Surg Case Rep 2017;3:99. [Crossref] [PubMed]
- Özkan B, Toker A. Catastrophes during video-assisted thoracoscopic thymus surgery for myasthenia gravis. Interact Cardiovasc Thorac Surg 2016;23:450-3. [Crossref] [PubMed]
- Shiono H, Inoue A, Tomiyama N, et al. Safer video-assisted thoracoscopic thymectomy after location of thymic veins with multidetector computed tomography. Surg Endosc 2006;20:1419-22. [Crossref] [PubMed]
- Natsag J, Tomiyama N, Inoue A, et al. Preoperative assessment of thymic veins on multidetector row CT: optimization of contrast material volume. Radiat Med 2007;25:202-10. [Crossref] [PubMed]
- Numanami H, Yano M, Yamaji M, et al. Thoracoscopic Thymectomy Using a Subxiphoid Approach for Anterior Mediastinal Tumors. Ann Thorac Cardiovasc Surg 2018;24:65-72. [Crossref] [PubMed]
- Ye B, Tantai JC, Ge XX, et al. Surgical techniques for early-stage thymoma: video-assisted thoracoscopic thymectomy versus transsternal thymectomy. J Thorac Cardiovasc Surg 2014;147:1599-603. [Crossref] [PubMed]
- McPhee A, Shaikhrezai K, Berg G. Is it safe to divide and ligate the left innominate vein in complex cardiothoracic surgeries?. Interact Cardiovasc Thorac Surg 2013;17:560-3. [Crossref] [PubMed]
- Wang HQ, Tian F, Wei M, et al. Preliminary evaluation and discussion of the safety of left innominate vein resection. J Thorac Dis 2020;12:438-47. [Crossref] [PubMed]
Cite this article as: Hussain K, Chen L, Gu Z, Fang W. Management of bleeding complications during thoracoscopic thymectomy. Mediastinum 2020;4:15.