
Thoracoscopic mediastinal tumor resection by subxiphoid approach—dual port thymectomy plus one (DPT+1)
Introduction
Recently, thoracoscopic subxiphoid approaches to mediastinal tumor such as single-port thymectomy (SPT) and dual-port thymectomy (DPT) using CO2 insufflation have been reported (1,2). The thoracoscopic approach has been demonstrated to have several advantages compared with the traditional median sternotomy approach, without compromising the oncological outcome, such as the following advantages: reduced intraoperative blood loss, lower risk of mediastinitis, earlier removal of chest drains, shorter hospital stay and superior cosmesis (3). Compared to the bilateral video-assisted thoracoscopic approach, thoracoscopic subxiphoid approaches are less invasive for chest wall paraesthesia and they allow prompt conversion to median sternotomy without posture change when needed (such as in the case of unexpected vascular injury) since the patient is in the supine position. However, SPT and DPT are technically demanding for novice surgeons since they require simultaneous insertion of surgical instruments and the thoracoscope into the same port, leading to interference between the surgical instruments and limitation of surgical view. To overcome these limitations, we propose a new surgical method, termed DPT plus one (DPT+1) (Figure 1).

Technique
The patient was positioned in an open-armed supine position and intubated with a double-lumen endotracheal tube for one-lung ventilation. First, a 3-cm vertical skin incision was made 1-cm caudal to the xiphoid process and the connective tissue between the xiphoid and the rectus abdominis was detached. The GelPOINT mini (Applied Medical, Rancho Santa Margarita, CA, USA) was fixed there as a utility port, and the two attached ports were inserted in GelPOINT mini platform. This utility port was used as a camera/assist port for the assistant. CO2 insufflation of the mediastinum was initiated at 8–10 mmHg to secure the surgical view. Next, the mediastinal pleura on the tumor located side was resected via the utility port using a LigaSure™ Maryland Jaw 37 cm (Covidien, Mansfield, MA, USA) and the thoracic cavity was opened. Two 5-mm ports at the 5th intercostal anterior axillary line and the 5th intercostal midclavicular line on the tumor located side were made by optical trocars (Medtronic, Minneapolis, MN, USA) while observing the insertion site via the thoracoscope. By using these two ports as access ports for the operator, we were able to completely separate the surgical access ports and the camera port added an accessory port for the assistant to avoid both interference between the surgical instruments and limitation of the surgical view.
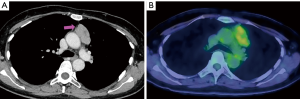
We present a case of a 53-year-old female without myasthenia gravis in which a 5-cm thymoma was resected by DPT+1 (Figure 2). Operation time: 97 min, blood loss: 10 mL (Figure 3). The patient had no postoperative complication and discharged at the 6th postoperative day.
Comments
Although SPT and DPT are markedly advantageous in various aspects for mediastinal tumor resection as described above, they are technically difficult for novice surgeons and may even be a challenging for the experienced surgeons. In particular, compared with DPT, SPT is technically demanding to be familiar with operating flexible clinch instruments. By simply adding one more intercostal port to DPT, DPT+1 separates the access ports for the operator and the camera port for the assistant to function independently, thereby allowing for a safer and easier surgery while taking advantage of the subxiphoid approach.
Our method might be feasible not only for simple mediastinal resections but also for extended thymectomies. When performing an extended thymectomy, it is crucial to visually identity the bilateral phrenic nerve in order to avoid surgical complications and to resect as much of the thymus as possible. Although Abdelnour-Berchtold et al. (5) reported on thoracoscopic thymectomy with intercostal ports from the right- or left-side approach in the supine position, with such approaches it is difficult to recognize the contralateral phrenic nerve visually. The subxiphoid approach clearly visualizes the bilateral phrenic nerve and allows easy dissection of the superior pole of the thymus. Furthermore, our method may provide advantages for more complicated cases, such as those involving pericardial invasion or lung infiltration since the independent dual access ports allows the operator to perform without interference between surgical instruments, therefore complex maneuvers such as suturing may even be achieved.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/med.2019.06.02). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committees and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Suda T, Hachimaru A, Tochii D, et al. Video-assisted thoracoscopic thymectomy versus subxiphoid single-port thymectomy: initial results†. Eur J Cardiothorac Surg 2016;49:i54-8. [PubMed]
- Suda T, Ashikari S, Tochii D, et al. Dual-port thymectomy using subxiphoid approach. Gen Thorac Cardiovasc Surg 2014;62:570-2. [Crossref] [PubMed]
- Weaver H, Ali JM, Jiang L, et al. Uniportal subxiphoid video-assisted thoracoscopic approach for thymectomy: a case series. J Vis Surg 2017;3:169. [Crossref] [PubMed]
- Ito A, Kaneda S, Shimamoto A, et al. We performed a thoracoscopic thymothymectomy on a patient with 5-cm thymoma by DPT+1. Asvide 2019;6:175. Available online: http://www.asvide.com/article/view/32328
- Abdelnour-Berchtold E, Perentes J, Krueger T, et al. Thoracoscopic thymectomy using a left-side approach. Multimed Man Cardiothorac Surg 2018; [Crossref] [PubMed]
Cite this article as: Ito A, Kaneda S, Shimamoto A, Takao M. Thoracoscopic mediastinal tumor resection by subxiphoid approach—dual port thymectomy plus one (DPT+1). Mediastinum 2019;3:26.


