
The value of mediastinoscopy in N staging of clinical N2 lung cancer
Introduction
Half a century has passed since mediastinoscopy was adopted for clinical application, and it has long been the “golden standard” for preoperative staging of mediastinal lymph nodes (1). In recent times, with the development of imageological and minimal invasive diagnostic techniques, the value of mediastinoscopy in lung cancer has diminished. Nonetheless, it still remains the most reliable method due to its high sensitivity and specificity. And this study was conducted to determine the value of mediastinoscopy in N staging of lung cancer with clinical N2 disease.
Methods
Patient selection and clinical characteristics
A total of 119 patients underwent mediastinoscopy for lymph node staging between September 1999 and April 2008 in the Department of Thoracic Surgery, Peking University People’s Hospital. Eighty-seven patients who were pre-operatively diagnosed N2 positive by imageological materials were deemed eligible for the study. Of the 87 patients eligible, 61 were suspected highly for lung cancer while 26 were definitively diagnosed with lung cancer. All 87 patients underwent chest radiography, chest computed tomography (CT), cytology, bacteriology, bronchoscopy, and other related examinations before operation. If their chest CT suggested enlargement of the ipsilateral mediastinal and/or subcarinal lymph nodes (short axis >1.0 cm), thymectomy was conducted for pathological staging. Ethics approval was not required as this is a retrospective non-invasive study.
Surgical technique
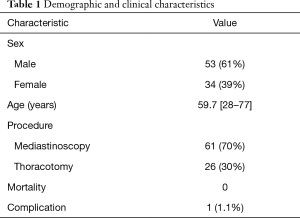
Demographic characteristics of the patients are listed in Table 1. Of the 87 eligible patients, 83 patients underwent standard cervical mediastinoscopies, and 4 underwent parasternal mediastinoscopies according to the position of the enlarged lymph nodes. All the patients were treated with general anesthesia, underwent single-lumen endotracheal intubation, and were placed in supine position with the head backward. During cervical mediastinoscopy, a cut was made at a distance of a finger’s width above the suprasternal notch with a length of about 3–4 cm. A dissection was then made to the trachea, after which a mediastinoscope was placed along the space both sides of the trachea. Next, the suspicious and/or enlarged paratracheal and subcarinal lymph node masses were explored and biopsied in order. The cut of parasternal mediastinoscopies was made at a distance of 2 cm parasternal at the level of the 2nd or 3rd rib with a length of about 4–5 cm; then, a dissection was made downwards along the substernal area, after which a mediastinoscope was placed along the pretracheal space, the mediastinal pleura and the nerves phrenicus of the operation side were pushed outwards with a narrow retractor, and the mediastinoscope was placed into the anterior mediastinum. Finally, the enlarged lymph nodes of group 5 and group 6 or enlarged anterior mediastinal lymph nodes were explored and biopsied. There was usually no need for post-operative drainage.
Full table
Results
Of the 87 patients eligible, 53 were male while 34 were female; the average age was 59.7 (range, 28–77) years old. After the mediastinoscopy, 61 patients proved to pathologically be N2 disease; the other 26 patients who were negative on mediastinoscopy were converted to thoracotomy, lobectomy, or wedge resection with mediastinal lymph node dissection. Of these patients, 24 proved pathologically negative, while 2 proved positive (false-negative by mediastinoscopy). The sensitivity, specificity, and accuracy of mediastinoscopy were 96.8%, 100%, and 97.7%, respectively.
Of all the mediastinoscopic procedures, there was no mortality, and the complication rate was 1.1%; only 1 patient suffered innominate artery injury, and the patient’s recovery was uneventful after median sternotomy patching.
Conclusions
Accurate staging plays an important role in the treatment selection and prognosis estimation of lung cancer, especially for those who are operable. At present, clinical N staging for lung cancer depends mostly on imageological examination; however, the accuracy of the existing imageological techniques (CT or PET-CT) is insufficient, as they have comparably high false-positive and false-negative rates. A large amount of research has shown that the false-positive rate of CT scan can be as high as 40% with the present diagnostic criteria (lymph nodes with a diameter more than 1 cm indicates lymph node metastasis). For example, the results of a review in 2007 revealed that of the 5,111 lung cancer patients who underwent CT scan to estimate N2 disease, 40% of the patients who were proven imageologically positive proved to be pathologically negative, while 40% of the patients who were proven imageologically negative proved to be pathologically positive; the sensitivity and specificity of the CT scans were 51% and 86% respectively (1). These results indicate that the estimation of CT scans may lead to over-diagnosis or missed diagnosis. Although the sensitivity, specificity, and accuracy of PET-CT scan is higher compared to CT, the same problem still exists. A study by Gonzalez-Stawinski et al. compared the value of PET-CT and mediastinoscopy in N staging for non-small cell lung cancer (NSCLC) in 202 patients who underwent mediastinoscopy after PET-CT scan; results showed that the sensitivity, specificity, and accuracy of the PET-CT scan were 64.4%, 77.1% and 74.3% respectively (2).
Thus, it has been a consensus worldwide that for lung cancer patients who are imageologically diagnosed with lymph nodes metastasis, mediastinoscopy should be conducted for N staging before a decision is made for treatment (3,4). This is not only effective for avoiding unnecessary exploratory thoracotomy, but also helpful in settling on treatment (5).
There are several techniques for the examination of mediastinal lymph node metastasis in lung cancer patients at present, such as mediastinoscopy, transthoracic needle aspiration (TTAN), transbronchial needle aspiration (TBNA), endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA), endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA), and video-assisted thoracoscopic surgery (VATS). Of these, mediastinoscopy still remains the standard technique for the mediastinal staging of lung cancer because of its high sensitivity and specificity.
In our study, of the 87 patients who were diagnosed with N2 disease by pre-operative imageological examination and received mediastinoscopy for N staging, 61 cases proved to be N2 disease on mediastinoscopy. The sensitivity, specificity, and accuracy of mediastinoscopy were 96.8%, 100%, and 97.7%, and higher than those of both CT and PET-CT scan. Detterbeck et al., Zwischenberger et al. and Annema et al. compared the sensitivity and specificity of the techniques mentioned above for the examination of mediastinal lymph node metastasis in lung cancer, and the results showed no statistical difference. As was mentioned above, TTAN, TBNA, and EUS-FNA are mainly used as screening methods before mediastinoscopy, or as supplements to reduce the use of mediastinoscopy (6-8). Several studies have shown that EBUS-TBNA has become an increasingly important technique in lung cancer diagnosis and N staging in recent years. EBUS-TBNA not only incurs less trauma, but also has a similar sensitivity and specificity compared to mediastinoscopy (9,10); thus, some studies have speculated that it may take the place of mediastinoscopy (11). However, clinical evidence of this replacement is not sufficient, especially in the form of relevant randomized controlled trials. Furthermore, it is unlikely that EBUS-TBNA will find broad clinical application due to its costly equipment, complicated technique, and lack of clinician familiarity with ultrasound. In conclusion, mediastinoscopy is still a highly effective and safe procedure for the mediastinal staging for lung cancer with clinical N2 disease.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors Marcin Zielinski and Qingdong Cao for the series “Mediastinoscopic Surgery” published in Mediastinum. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/med.2019.05.03). The series “Mediastinoscopic Surgery” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethics approval and written informed consent were not required as this is a retrospective non-invasive study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Silvestri GA, Gould MK, Margolis ML, et al. Noninvasive staging of non-small cell lung cancer: ACCP evidence-based clinical practice guidelines (2nd edition). Chest 2007;132:178s-201s.
- Gonzalez-Stawinski GV, Lemaire A, Merchant F, et al. A comparative analysis of positron emission tomography and mediastinoscopy in staging non-small cell lung cancer. J Thorac Cardiovasc Surg 2003;126:1900-5. [Crossref] [PubMed]
- Wu YL, Jiang GL, Liao ML, et al. Chinese consensus on treatment of III A N2 non-small cell lung cancer. J Evidence-Based Med 2008;8:113-117.
- NCCN. Non-Small-Cell Lung Cancer Practice Guidelines. Practice Guidelines in Oncology v.1, 2007.
- Wang J, Zhao H. Mediastinoscopy and the value of mediastinoscopy in staging of lung cancer. Zhonghua Zhong Liu Za Zhi 2002;24:74-6. [PubMed]
- Detterbeck FC, Jantz MA, Wallace M, et al. Invasive mediastinal staging of lung cancer: ACCP evidence-based clinical practice guidelines (2nd edition). Chest 2007;132:202s-220s.
- Zwischenberger JB, Savage C, Alpard SK, et al. Mediastinal trans- thoracic needle and core lymph node biopsy: Should it replace mediastinoscopy? Chest 2002;121:1165-70. [Crossref] [PubMed]
- Annema JT, Versteegh MI, Veselic M, et al. Endoscopic ultrasound added to mediastinoscopy for preoperative staging of patients with lung cancer. JAMA 2005;294:931-6. [Crossref] [PubMed]
- Herth FJ, Eberhardt R, Vilmann P, et al. Real-time endobronchial ultrasound guided transbronchial needle aspiration for sampling mediastinal lymph nodes. Thorax 2006;61:795-8. [Crossref] [PubMed]
- Vincent BD, El-Bayoumi E, Hoffman B, et al. Real-time endobronchial ultrasound-guided transbronchial lymph node aspiration. Ann Thorac Surg 2008;85:224-30. [Crossref] [PubMed]
- Ernst A, Anantham D, Eberhardt R, et al. Diagnosis of mediastinal adenopathy-real-time endobronchial ultrasound guided needle aspiration versus mediastinoscopy. J Thorac Oncol 2008;3:577-82. [Crossref] [PubMed]
Cite this article as: Xiao R, Li Y, Zhao H, Li X, Wang X, Wang J. The value of mediastinoscopy in N staging of clinical N2 lung cancer. Mediastinum 2019;3:23.


