
Management of incidental anterior mediastinal lesions: summary of relevant studies
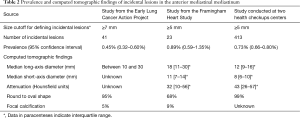
Mediastinal lesions include a variety of benign and malignant diseases. Half of these lesions are located in the anterior mediastinum, mostly originating from the thymus (1). With the increasing use of chest computed tomography (CT) imaging in clinical practice (2) and lung cancer screening (3), asymptomatic incidental anterior mediastinal lesions are more frequently encountered. Three studies have dealt with the prevalence of incidental nodular lesions in the anterior mediastinum (4-6) (Table 1). The first was from the Early Lung Cancer Action Project (ELCAP) (4), the second utilized data from the Framingham Heart Study (5), and the third was conducted at two health checkup centers affiliated with a tertiary academic hospital (6). The number of participants ranged from 2,571 to 56,358, and the age and sex distribution was similar across the studies. However, ever-smokers were more prevalent in the ELCAP study (4) than in the others (5,6). Most participants in the three studies underwent thin-slice CT scans (1.25 mm or thinner), but in the ELCAP study (4), the slice thickness was 2.5 or 10 mm in the baseline CT images of 32% of the participants.

Full table
The prevalence of incidental nodular lesions in the anterior mediastinum in these studies ranged from 0.45% to 0.89% (Table 1). The ELCAP study reported a prevalence of 0.45% (95% CI, 0.32–0.60%; 41 of 9,263 participants) (4). The Framingham Heart Study reported a prevalence of 0.89% (95% CI, 0.59–1.35%; 23 of 2,571 participants) (5). Lastly, among 56,358 healthy participants who underwent a low-dose chest CT scan as part of their health checkups, the prevalence was 0.73% (6). The variation in the prevalence across these studies seems to have been due to differences in the study population, CT slice thickness, and lesion definition. The ELCAP study (4) applied a cutoff of a short-axis diameter of 7 mm or larger to identify incidental nodular lesions, whereas the other two studies (5,6) adopted a cut-off of 5 mm or larger.
One study (6) reported that the prevalence of incidental lesions increased with age, with the following distribution: 25–34 years, 0.40%; 35–44 years, 0.47%; 45–54 years, 0.58%; 55–64 years, 0.89%; 65–74 years, 1.26%; >75 years, 1.44% (P<0.001). The prevalence of incidental lesions was not associated with sex, cigarette smoking, or body mass index (5,6). Patients with a history of malignancy had incidental lesions more frequently than those with no such history (2.06% versus 0.72%; P=0.005) (6). A similar tendency of the increased thymoma risk following other malignancies was found in the SEER data (standardized incidence ratio, 1.3; 95% CI, 1.0–1.7), despite the lack of significant association between particular cancer and thymoma (7).
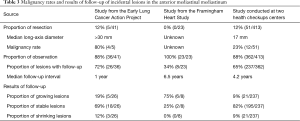
Most incidentally-detected lesions in the anterior mediastinum were small nodules with a soft tissue appearance (Table 2). The long-axis diameter of the lesions was mostly between 10 and 30 mm (4), with a median value of 12 to 18 mm (5,6). The shape of the lesions was typically round to oval. The mean CT attenuation of the lesions was 32 to 43 Hounsfield units (5,6), which corresponds to soft tissue attenuation. Focal calcifications within the lesions were rare (4,5). In other words, most lesions had CT features indistinguishable from those of thymic epithelial tumors on precontrast CT images.
Full table
The distribution of pathologies in anterior mediastinal lesions varies according to age and sex (8). Because incidental anterior mediastinal lesions are primarily encountered on screening chest CT scans in patients in their 50–70 s, thymic epithelial tumors are a main concern. Malignant lesions seem to be more prevalent among larger lesions in the anterior mediastinum, especially among those measuring 30 mm or larger. More specifically, thymic epithelial tumors are mainly responsible for larger lesions, whereas smaller lesions are primarily benign thymic cysts (Table 3). In two of the three studies, a small subset of the detected lesions (12% in each study) underwent surgical resection (4,6). In the ELCAP study (4), all five lesions larger than 30 mm were resected, and four of those lesions were malignant (proportion of malignancy, 80%), including three thymomas and one thymic carcinoma. The benign lesion was a thymic cyst. In contrast, in the study conducted at health checkup centers (6), 51 lesions were resected, of which 12 were malignant (proportion of malignancy, 23%): 11 thymic epithelial tumors and one case of non-small cell lung cancer. Among the 39 cases of benign disease, most were benign cysts in the thymic bed, including 32 thymic cysts and four bronchogenic cysts. The median long-axis diameter of the resected lesions was 17 mm. The discrepancy in the proportion of malignancy between the two studies may have been due to the different diameter of the resected lesions. Indeed, a subgroup analysis in the latter study showed that the proportion of malignancy was much higher in lesions larger than 20 mm than in those 20 mm or smaller (50% versus 13.5%; P=0.011).
Full table
Incidentally-detected thymic epithelial tumors had favorable outcomes when resected. One study (6) provided the detailed characteristics of the resected thymic epithelial tumors in 11 cases with a median long-axis diameter of 21 mm. Of the 11 resected thymic epithelial tumors, five were thymic carcinomas, 10 were stage I or II according to the Masaoka-Koga staging system, and all the lesions were completely resected without recurrence during a median follow-up of 5.6 years. Despite the small number of cases, the lack of recurrence of the incidental lesions is strikingly different from the recurrence rates of 11–13% that have been reported for clinically-detected thymic epithelial tumors (9), with a particularly higher recurrence rate for thymic carcinoma (10).
In the study conducted at health checkup centers (6), 12% of the detected lesions were resected, resulting in a prevalence of thymic epithelial tumors (0.02%) that was twice as high (standardized prevalence ratio, 2.04) as the expected prevalence (0.01%) based on national cancer statistics. Indeed, incidental thymic epithelial tumors seem fairly prevalent. A postmortem study also reported a higher prevalence of thymic epithelial tumors (0.18%; 57 of 31,000) than would be predicted based on the national cancer statistics (11). It remains unclear whether the surgical resection of incidental thymic epithelial tumors leads to overdiagnosis or whether the resection of the lesions results in a survival benefit in patients with thymic epithelial tumors.
In all three studies (4-6), 88–100% of the incidentally detected lesions were managed by close observation with follow-up CT scans, although the proportion of patients receiving follow-up and the follow-up interval were inhomogeneous across the studies (Table 3). A majority of the incidental lesions were stable during follow-up (4,6), except for the study based on the Framingham Heart Study (5), which reported a growth in 75% of lesions over a longer follow-up of 6.5 years. Nevertheless, even in the latter study, the growing lesions measured approximately 30 mm on the follow-up CT scans (median long-axis diameter, 27 mm; range, 10–38 mm). The median follow-up duration to notice an increase was quite long (3.7 years) and the median increase of the longest diameter was 3 mm (6). Thus, incidental lesions seem mostly stable; some lesions do grow over multi-year follow-up, but their growth is indolent.
Conservative management with follow-up is recommended for incidental lesions. Nevertheless, regular follow-up may not be the sole solution, as long-term repeated follow-up is required to detect any increase or decrease in lesion size and neither interval growth nor a lack of growth during follow-up can guarantee either malignancy or benignity (6). Non-invasive imaging studies such as thoracic magnetic resonance imaging (MRI) can be helpful for further characterizing incidental anterior mediastinal lesions, especially thymic cysts (12), and for alleviating patients’ anxiety. Indeed, state-of-art thoracic MRI offers excellent contrast resolution, which enables various tissue characteristics of anterior mediastinal lesions to be depicted without motion artifacts (13).
In conclusion, the prevalence of incidental anterior mediastinal lesions ranges from 0.45% to 0.89%, and many of these lesions are suspected to be benign. A conservative patient-tailored approach with follow-up is required, and thoracic MRI can be used as a supplementary tool for the management of the lesions.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors Mirella Marino and Brett W. Carter for the series “Dedicated to the 9th International Thymic Malignancy Interest Group Annual Meeting (ITMIG 2018)” published in Mediastinum. The article has undergone external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/med.2019.03.01). The series “Dedicated to the 9th International Thymic Malignancy Interest Group Annual Meeting (ITMIG 2018)” was commissioned by the editorial office without any funding or sponsorship. The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Strollo DC, Rosado de Christenson ML, Jett JR. Primary mediastinal tumors. Part 1: tumors of the anterior mediastinum. Chest 1997;112:511-22. [Crossref] [PubMed]
- Smith-Bindman R, Miglioretti DL, Johnson E, et al. Use of diagnostic imaging studies and associated radiation exposure for patients enrolled in large integrated health care systems, 1996-2010. JAMA 2012;307:2400-9. [Crossref] [PubMed]
- Moyer VA, Force USPST. Screening for lung cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 2014;160:330-8. [PubMed]
- Henschke CI, Lee IJ, Wu N, et al. CT screening for lung cancer: prevalence and incidence of mediastinal masses. Radiology 2006;239:586-90. [Crossref] [PubMed]
- Araki T, Nishino M, Gao W, et al. Anterior Mediastinal Masses in the Framingham Heart Study: Prevalence and CT Image Characteristics. Eur J Radiol Open 2015;2:26-31. [Crossref] [PubMed]
- Yoon SH, Choi SH, Kang CH, et al. Incidental Anterior Mediastinal Nodular Lesions on Chest CT in Asymptomatic Subjects. J Thorac Oncol 2018;13:359-66. [Crossref] [PubMed]
- Engels EA. Epidemiology of thymoma and associated malignancies. J Thorac Oncol 2010;5:S260-5. [Crossref] [PubMed]
- Carter BW, Marom EM, Detterbeck FC. Approaching the patient with an anterior mediastinal mass: a guide for clinicians. J Thorac Oncol 2014;9:S102-9. [Crossref] [PubMed]
- Tomaszek S, Wigle DA, Keshavjee S, et al. Thymomas: review of current clinical practice. Ann Thorac Surg 2009;87:1973-80. [Crossref] [PubMed]
- Girard N, Ruffini E, Marx A, et al. Thymic epithelial tumours: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2015;26:v40-55. [Crossref] [PubMed]
- Mirra M, Zanella M, Bussani R, et al. Intrapericardial thymoma: report of two incidental autopsy cases and review of the literature. Arch Pathol Lab Med 1997;121:59-63. [PubMed]
- Carter BW, Okumura M, Detterbeck FC, et al. Approaching the patient with an anterior mediastinal mass: a guide for radiologists. J Thorac Oncol 2014;9:S110-8. [Crossref] [PubMed]
- Ackman JB. MR Imaging of Mediastinal Masses. Magn Reson Imaging Clin N Am 2015;23:141-64. [Crossref] [PubMed]
Cite this article as: Yoon SH. Management of incidental anterior mediastinal lesions: summary of relevant studies. Mediastinum 2019;3:9.


