Lymph node dissection in thymic malignancies
Lymph node metastasis is not uncommon and an important clinical parameter in thymic malignancies. It is consistently reported that lymph node metastasis is a poor prognostic factor in thymic malignancies (1-4). Original Masaoka stage classification system and latest International Association for the Study of Lung Cancer (IASLC)/International Thymic Malignancy Interest Group (ITMIG) stage classification system for thymic malignancies classify lymph node metastasis as stage IV (5,6). Understandings, however, about the details of lymph node metastasis in thymic malignancies such as incidence, lymphatic pathway, method of lymph node dissection (LND), and the benefit of diagnosis of lymph node metastasis are extremely limited until now.
The ChART study about lymph node metastases in thymic malignancies by Gu et al. is the latest and largest series about this subject which evaluated 1,617 surgical cases (3). All lymph node metastases in this study were diagnosed pathologically with surgical specimens. In ChART study, incidence of lymph node metastasis had significant relation with World Health Organization (WHO) histologic subtype and T stage. There was no lymph node metastasis in type A/AB/B1. Lymph node metastasis rate were 1.3% in type B2/B3, 7.9% in type C, and 16.7% in neuroendocrine thymic tumors. Lymph node metastasis rate were 0.2% in T1, 6.9% in T2, 8.5% in T3, and 7.4% in T4. Nodal metastasis was independent prognostic factor in thymic carcinoma but was only marginally significant in thymoma (3). The results of ChART study are consistent with previous studies. Japanese multi-institutional study, Korean single institutional study and SEER data analyses from USA also showed WHO histologic subtype and tumor invasiveness (T stage) are factors for lymph node metastasis and lymph node metastasis is a poor prognostic factor (1,2,4). The ChART study, however, has limitations as like other studies. Limitations are small number of subgroup due to rarity of thymic malignancies, heterogeneity between histologic subtypes, lack of standardized LND strategy, no detailed data about LND and inconsistent adjuvant treatment in patients with lymph node metastasis. The most crucial limitation is that no standardized protocol of LND ever has been applied in thymic malignancies. The IASLC/ITMIG staging project for thymic malignancies also failed to performed meaningful analysis about nodal metastasis because of paucity of available detailed data (6). Thus, accumulation of data under standardized LND protocol is the only realizable and exigent task at present. Without organized large scale data, this issue will be remain controversial forever. LND is recommended in other thoracic malignancies to achieve more accurate pathologic stage which enables precise prediction of prognosis and affords chance to perform possibly beneficial adjuvant treatment (7,8). Furthermore, removal of lymph node with metastasis can improve loco-regional disease control.
The first step to building an organized data for lymph node metastasis is using a universal and systematic lymph node map. Yamakawa had proposed a nodal classification system for thymic malignancies (9). But, the definition of that system was not minute. Recently, ITMIG proposed a systematic lymph node map for thymic malignancies with precise explanation (10). In ITMIG lymph node map, anterior regional nodal group including low anterior cervical and anterior mediastinal nodes are classified as N1 station. Deep regional nodes including deep cervical, internal mammary and middle mediastinal nodes are classified as N2 station. One of unique changes in ITMIG lymph node map is classifying paraaortic node group (IASLC lung cancer lymph node map station #6) as N1 station. N3 station does not exist and all other node metastases are classified as M1 stage in ITMIG lymph node map (10). The ITMIG lymph node map should be used as a standard lymph node map for clinical practice and research of thymic malignancies because using common language is the starting point for the communication and collaboration among world-wide researchers studying this rare disease.
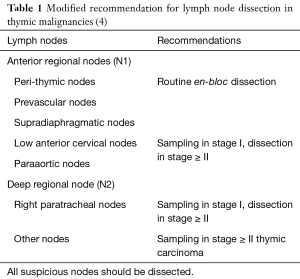
Another issue is ensuring quality of LND. The extent of LND and the number of dissected lymph node are generally used quality measures of LND in other thoracic malignancies. The extent and the number of dissected node would affect the accuracy of pathologic staging in thymic malignancies as proved in lung cancer and esophageal cancer (7,8). The ChART study and other large scale studies contain no detailed data about the extent of LND and the number of dissected lymph node. In SEER database studies, only median number of evaluated lymph nodes were reported and further meaningful analyses were impossible (2). Our group reported two studies about the extent of LND and the number of dissected lymph nodes in thymic malignancy patients who underwent intentional LND. We divided pathologic N0 thymic carcinoma into pN0a (dissected lymph nodes ≤10) and pN0b (dissected lymph nodes >10), then compared prognoses of two groups with Nx (no LND) and pN1 groups. Prognoses of pNx and pN0a groups were similar, and the prognoses of both groups were intermediate between the pN0b and pN1 groups. This finding suggests more than 10 nodes should be evaluated to predict prognosis accurately in thymic carcinoma (11). As like in ChART study, our study also showed WHO histologic subtype and tumor invasiveness were factors for the lymph node metastasis in thymic malignancies. Rate of lymph node metastasis in T2/3 stage was 37.5% whereas only 1% of T1 stage had lymph node metastasis. Nodal metastasis rate was 5.1% in thymoma and 25% in thymic carcinoma. There was no nodal metastasis in 101 WHO type A/AB/B1. An important finding of our study is frequent metastasis to the right paratracheal lymph nodes group regardless of tumor location. Six out of 7 pN2 patients had metastases at right paratracheal lymph nodes (4). This phenomenon closely accord with the findings of anatomical study by Murakami et al.(12) The right paratracheal lymph node group plays important role in the lymphatic pathway of thymic malignancies and should be dissected in high grade histology or locally advanced thymic malignancies. ITMIG already proposed recommendation about LND strategy for thymic malignancies in 2011. ITMIG recommended removal of any suspicious nodes, removal of adjacent nodes and anterior mediastinal nodes in stage I and II thymomas, systematic anterior mediastinal node dissection and systematic sampling of appropriate intrathoracic nodes in stage III thymomas and at least a systematic sampling of anterior mediastinal, intrathoracic, supraclavicular, and lower cervical nodes for thymic carcinomas (if the diagnosis is suspected or known) (13). This recommendation was devised based on Yamakawa-Masaoka nodal staging system and available data at that time. In the meantime, new lymph node map and new stage classification system have replaced the former standards and more information about pattern of nodal metastasis have been accumulate. Thus, modification of ITMIG recommendation considering recent changes is necessary to improve quality LND for the future studies. We have proposed a modified recommendation based on ITMIG lymph node map and IASLC/ITMIG stage classification system for thymic malignancies and put emphasis on the dissection of right paratracheal lymph node group (Table 1) (4).
Lymph node metastasis is an important parameter in thymic malignancies. But current understandings about lymph node metastasis in thymic malignancies is substantial. LND is the only realizable method to achieve deep knowledge of lymph node metastasis in thymic malignancies and should be performed on the basis of new standards.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned and reviewed by Section Editor Dr. Zhuoqi Jia (Thoracic Department, the First Affiliated Hospital of Xi’an Jiaotong University, Xi’an, China).
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/med.2017.08.02). The author has no conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kondo K, Monden Y. Lymphogenous and hematogenous metastasis of thymic epithelial tumors. Ann Thorac Surg 2003;76:1859-64; discussion 1864-5.
- Weksler B, Pennathur A, Sullivan JL, et al. Resection of thymoma should include nodal sampling. J Thorac Cardiovasc Surg 2015;149:737-42. [Crossref] [PubMed]
- Gu Z, Wei Y, Fu J, et al. Lymph node metastases in thymic malignancies: a Chinese Alliance for Research in Thymomas retrospective database analysisdagger. Interact Cardiovasc Thorac Surg 2017;25:455-61. [PubMed]
- Hwang Y, Park IK, Park S, et al. Lymph Node Dissection in Thymic Malignancies: Implication of the ITMIG Lymph Node Map, TNM Stage Classification, and Recommendations. J Thorac Oncol 2016;11:108-14. [Crossref] [PubMed]
- Masaoka A, Monden Y, Nakahara K, et al. Follow-up study of thymomas with special reference to their clinical stages. Cancer 1981;48:2485-92. [Crossref] [PubMed]
- Kondo K, Van Schil P, Detterbeck FC, et al. The IASLC/ITMIG Thymic Epithelial Tumors Staging Project: proposals for the N and M components for the forthcoming (8th) edition of the TNM classification of malignant tumors. J Thorac Oncol 2014;9:S81-7. [Crossref] [PubMed]
- Lardinois D, De Leyn P, Van Schil P, et al. ESTS guidelines for intraoperative lymph node staging in non-small cell lung cancer. Eur J Cardiothorac Surg 2006;30:787-92. [Crossref] [PubMed]
- Rizk NP, Ishwaran H, Rice TW, et al. Optimum lymphadenectomy for esophageal cancer. Ann Surg 2010;251:46-50. [Crossref] [PubMed]
- Yamakawa Y, Masaoka A, Hashimoto T, et al. A tentative tumor-node-metastasis classification of thymoma. Cancer 1991;68:1984-7. [Crossref] [PubMed]
- Bhora FY, Chen DJ, Detterbeck FC, et al. The ITMIG/IASLC Thymic Epithelial Tumors Staging Project: A Proposed Lymph Node Map for Thymic Epithelial Tumors in the Forthcoming 8th Edition of the TNM Classification of Malignant Tumors. J Thorac Oncol 2014;9:S88-96.
- Park IK, Kim YT, Jeon JH, et al. Importance of lymph node dissection in thymic carcinoma. Ann Thorac Surg 2013;96:1025-32; discussion 1032. [Crossref] [PubMed]
- Murakami G, Sato T, Takiguchi T. Topographical anatomy of the bronchomediastinal lymph vessels: their relationships and formation of the collecting trunks. Arch Histol Cytol 1990;53:219-35. [Crossref] [PubMed]
- Detterbeck FC, Moran C, Huang J, et al. Which way is up? Policies and procedures for surgeons and pathologists regarding resection specimens of thymic malignancy. J Thorac Oncol 2011;6:S1730-8. [Crossref] [PubMed]
Cite this article as: Park IK. Lymph node dissection in thymic malignancies. Mediastinum 2017;1:4.