
The hemiclamshell approach to bulky cervico-mediastinal lesions: how to do it
Highlight box
Surgical highlights
• The hemiclamshell incision is a combination of partial median sternotomy and anterolateral thoracotomy, allowing excellent exposure of mediastinum, one pleural cavity and the neck. It can be used for superior sulcus tumors with mediastinal involvement or to resect bulky mediastinal lesions or lesions requiring cervical, mediastinal and pleural exposure.
What is conventional and what is novel/modified?
• Internal mammary vessels have to be carefully isolated, ligated and transected; this part of the procedure can be difficult, in the case of narrow intercostal spaces or previous radiotherapy.
• Mechanical vascular stapling allows safer, easier and faster management of mammary vessels.
What is the implication, and what should change now?
• Hemiclamshell is an appropriate approach in the case of bulky cervico-mediastinal lesions, not suitable for a minimally invasive approach. It is superior to standard sternotomy or thoracotomy alone when neck, mediastinum and one pleural cavity should be properly explored.
Introduction
Background
The hemiclamshell approach has rarely been used since the introduction to cardiac and thoracic surgery of longitudinal median sternotomy and the significative advances in minimally invasive cardio-thoracic surgery. However, in rare clinical conditions, as in bulky, space-occupying masses extending from the neck to the mediastinum and one pleural cavity, the hemiclamshell incision makes it possible to obtain complete exposure and an excellent surgical field for a safer excision (1).
Rationale
Standard median sternotomy provides excellent exposure of the mediastinum and the neck, in this case by starting the incision a couple of centimeters above the sternal manubrium; on the contrary it does not offer a proper view of the pleural cavities when they need to be extensively approached to resect huge masses, to safely perform lung resections and preserve many structures such as phrenic nerves, jugulo-subclavian venous confluence, aortic arch and supra-aortic vessels and superior vena cava. On the contrary antero-lateral thoracotomy offers an excellent view of the thoracic cavity but does not allow proper exposure of the entire mediastinum and mainly the neck, which is usually involved in the case of huge mediastinal masses.
The combination of both, resulting in the hemiclamshell approach, provides excellent exposure of neck, mediastinum and one pleural cavity, thus offering an excellent view in the case of bulky lesions extending from the neck to the mediastinum and one pleural cavity.
Objective
The objective of this paper is to describe the standard steps for performing a hemiclamshell incision by using modern devices and technology which contribute to make this procedure easier, faster and safer. We present this article in accordance with the SUPER reporting checklist (available at https://med.amegroups.com/article/view/10.21037/med-23-36/rc).
Preoperative preparations and requirements
The hemiclamshell approach can be adopted to manage bulky mediastinal lesions as well as superior sulcus tumors (Pancoast tumors) with mediastinal involvement (2). From the oncologic point of view, in the case of primary lung cancer, whole body computed tomography (CT) and positron emission tomography (PET) have to be performed to obtain proper preoperative staging. Magnetic resonance imaging (MRI) may be indicated in the case of vascular infiltration to better define operative strategy. In the case of primary mediastinal tumors, both PET and CT scans may be required, depending on the type of histology; whenever possible, preoperative histology should be obtained, particularly when extended resection with closer structure sacrifice is expected. In the case of suspected cardiac infiltration, preoperative cardiac MRI or cardiac CT can effectively contribute to proper preoperative resectability evaluation (3). Functional assessment of cardio-respiratory function should be tailored on the planned extent of the resection: in the case of planned pneumonectomy, spirometry, perfusion scanning and cardiopulmonary exercise testing are recommended. Due to the complexity of clinical scenarios usually involving cardiovascular and thoracic structures, these procedures should only be performed in carefully selected and experienced centers with a solid vascular, cardiac and thoracic background. Although these procedures can usually be completed without any cardiovascular support, cardiopulmonary bypass should be available, particularly in the case of suspected cardiovascular infiltration. As postoperative complications can frequently arise after extended resection, an experienced multidisciplinary team should always be available for prompt management (4). All procedures performed in this study were in accordance with the ethical standards of the institutional research committee and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the publication of this article and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Step-by-step description
The patient is usually placed in the supine position with the arm bilaterally abducted at 90°; this is the favorite decubitus when only mediastinal resection is planned. If an anatomic pulmonary resection is expected, it is preferable to have a 30° rotation towards the opposite side of the thoracotomy; this will allow better exposure of the pulmonary hilum, in particular the lower one on the left side, if pneumonectomy or major pulmonary resection is planned.
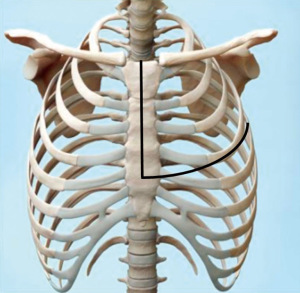
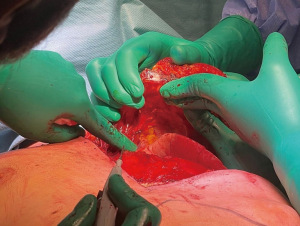
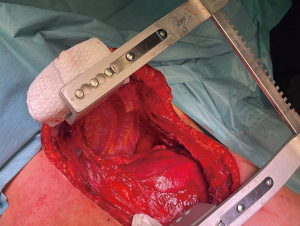
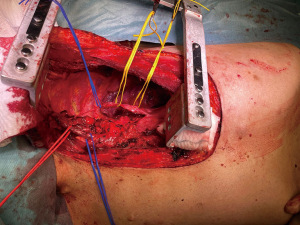
Antero-lateral thoracotomy should always be performed first. This approach allows preliminary exploration of the surgical field; once the resection is judged feasible, partial median sternotomy is performed. Antero-lateral thoracotomy is usually performed in the 4th intercostal space; in some very selected cases it is possible to enter the pleural cavity through the 3rd intercostal space while, on the contrary, it is not useful to enter the 5th intercostal space. Serratus anterior muscle fibers are dissected while pectoralis major fibers are disinserted form the rib; latissimus dorsi muscle fibers are usually not involved. When the antero-lateral thoracotomy is performed in the 4th intercostal space, the distal third of the body of the sternum is preserved and the sternotomy in extended from the jugulum to the 4th chondro-sternal joint. Before performing the sternotomy, the retrosternal space should be gently dissected with the fingers from the antero-lateral thoracotomy in order to create a retrosternal tunnel where the sternal saw can easily proceed without touching bulky and easily bleeding masses. Before starting the sternotomy, the mammary vessels must be identified and divided to allow a sequential transverse hemisternotomy. When the intercostal space is very narrow—or in the case of previous mediastinal radiotherapy—mammary vessel isolation, ligation and sectioning might be difficult; in this case we recommend a gross isolation of the mammary pedicle and then a mass sectioning using a mechanical vascular stapler (Figure 1). Sternotomy is then performed from the jugulum to the 4th chondro-sternal joint; the sternal saw is gently retracted and transverse hemisternotomy is then performed from the anterior edge of the antero-lateral thoracotomy to the midline of the sternum. This results in a sternocostal flap which is easily retracted and then pushed upwards to expose the pleuro-mediastinal cavity. Some soft adhesions are usually found between the pericardial fat and the posterior aspect of the sternocostal flap and should be carefully coagulated and dissected to maximize proper flap mobilization and cavity exposure (Figure 2). A Finochietto retractor is placed with the upper branch under the tip of the sternocostal flap and the lower one above the 5th chondro-sternal joint (Figure 3). This approach makes it possible to safely isolate the jugulo-subclavian confluence on both sides, the innominate vein on the left side, the superior vena cava on the right side, the aortic arch, the left subclavian artery and the left carotid artery on the left side, the aortic arch and the innominate artery on the right side; both the phrenic nerves can be effectively isolated and preserved when free from tumor infiltration (Figure 4). Once the resection is accomplished, both the antero-lateral thoracotomy and the sternotomy are routinely closed. We prefer absorbable stitches for the sternum rather than titanium ones, while two single standard stitches are enough for closing the thoracotomy. We recommend one or two chest drainages for draining the pleural cavity and one drainage for the retrosternal space. Care should be taken not to devascularize the skin to avoid skin flap necrosis at the confluence of the sternotomy and thoracotomy (Figure 5). Long term results are satisfactory and chest wall stability as well as arm mobility are fully preserved.
Postoperative considerations and tasks
Depending on the extent of the resection, intensive care unit (ICU) might be suggested after this approach. Daily post-operative chest X-ray is strongly recommended as well as careful chest drainage management. Drainage suction may be applied, depending on type and extent of resection to optimize lung re-expansion. Due to the extent of the incisions, we would rather suggest intravenous (I.V.) analgesia rather than topic approach (e.g., paravertebral block).
Tips and pearls
We suggest starting the procedure by always performing thoracotomy first: this allows proper exploration and confirms resectability; only after a complete thoracic cavity assessment has been performed, including the absence of pleural carcinosis, should sternotomy proceed.
Use vascular stapling for mammary vessel ligations; it is faster and safer, particularly in the case of very narrow intercostal spaces or after chest wall radiotherapy which makes vessels more fragile and difficult to isolate.
Optimize mediastinal exploration by positioning the patient with a slight bending in the subscapular regions, without excessive tension in order to prevent post-operative back pain. We recommend bilateral 90° abduction of both arms to easily access both pleural cavities, if needed.
Discussion
Surgical highlights
The hemiclamshell approach consists of a combination of partial median sternotomy and antero-lateral thoracotomy in the 4th intercostal space. It provides excellent exposure of the neck, mediastinum and one pleural cavity; its peculiar indications are bulky cervico-mediastinal tumors extending into one pleural cavity or anterior Pancoast tumors or primary tumors of the lung with mediastinal involvement, in this case more frequently observed on the left side. Consisting of two incisions, it is not—of course—a limited approach but, when correctly performed, post-operative pain and subsequent pulmonary function impairment can be successfully controlled by a proper therapy which relies on I.V. analgesia rather than epidural/peridural approaches because of the extent of the incisions.
Strengths and limitations
The main strength of this approach is the wide surgical field resulting from the combination of the two incisions; in particular on the left side, it allows full control of all vascular, neurological and pulmonary structures; on the other hand, it is a very aggressive approach and its indications should be limited to bulky lesions not amenable to safer management by less aggressive approaches.
Comparison with other surgical techniques and research
When compared to sternotomy alone or anterior thoracotomy alone, the hemiclamshell approach is superior in terms of overall view and safer control of all the structures which can be infiltrated by bulky mediastinal lesions; on the other hand, it should be considered only in the case of clear protrusion towards one of the pleural cavities and should not be adopted in the case of pure median lesions.
In fact, due to the sterno-costal flap—which is typically elevated in this approach—the uninvolved pleural cavity is not easily accessible and there is no way to further expand sternal divarication. Minimally invasive approaches—such as video-assisted, robot-assisted or sub-xiphoid—represent significantly less invasive approaches but cannot be considered in the case of bulky lesions invading neck, mediastinum and pleural structures.
Nevertheless, due to the rarity of the tumors requiring this kind of approach, there are no randomized prospective controlled trials comparing these techniques and a proper approach should be based on the volume and location of the lesion to be resected as well as on the surgeon’s experience (5-10).
Implications and recommended actions
Although the vast majority of mediastinal lesions can now be approached by minimally invasive techniques, the hemiclamshell incision still plays a pivotal role in the case of bulky lesions involving cervical, mediastinal and pleural cavities. Decision criteria for choosing the best approach rely not only on the dimensions of the target lesion or on the infiltration of close vital structures but also on the histology of the lesion to be resected, on preoperative induction treatments, on the clinical conditions of the patient and last—but not least—on the surgeon’s and the center’s experience. In the case of cardiac or great vessel involvement, the procedure should be performed in experienced high-volume centers with the availability of cardio-pulmonary bypass (CPB), extra-corporeal membrane oxygenator (ECMO) or venous shunts (11,12). In our personal experience, in the last five cases performed, we had one case of haemothorax.
Conclusions
Although the vast majority of mediastinal lesions can now be approached by minimally invasive techniques, the hemiclamshell incision still plays a pivotal role in the case of bulky lesions involving cervical, mediastinal and pleural cavities. It consists of a combination of subtotal median vertical sternotomy and antero-lateral thoracotomy in the 4th intercostal space, providing excellent exposure of the neck, mediastinum and one pleural cavity.
Acknowledgments
The English text was edited by Susan Jane West.
Funding: This work was partially supported by the Italian Ministry of Health with “Ricerca Corrente”, “5 × 1000” funds.
Footnote
Reporting Checklist: The authors have completed the SUPER reporting checklist. Available at https://med.amegroups.com/article/view/10.21037/med-23-36/rc
Peer Review File: Available at https://med.amegroups.com/article/view/10.21037/med-23-36/prf
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://med.amegroups.com/article/view/10.21037/med-23-36/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional research committee and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the publication of this article and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Saad H, Van Niekerk FN, Kadlec J. Hemiclamshell approach for left pneumonectomy. Multimed Man Cardiothorac Surg 2022; [Crossref] [PubMed]
- Petrella F, Leo F, Veronesi G, et al. "Salvage" surgery for primary mediastinal malignancies: is it worthwhile? J Thorac Oncol 2008;3:53-8. [Crossref] [PubMed]
- Chianca V, Albano D, Messina C, et al. An update in musculoskeletal tumors: from quantitative imaging to radiomics. Radiol Med 2021;126:1095-105. [Crossref] [PubMed]
- Cardinale D, Cosentino N, Moltrasio M, et al. Acute kidney injury after lung cancer surgery: Incidence and clinical relevance, predictors, and role of N-terminal pro B-type natriuretic peptide. Lung Cancer 2018;123:155-9. [Crossref] [PubMed]
- Machboua A, Thumerel M, Hustache-Castaing R, et al. Cervicotomy using a hemi-clamshell approach for a rare enlarged substernal goitre. Interact Cardiovasc Thorac Surg 2022;35:ivac056. [Crossref] [PubMed]
- Wang S, Chen Z, Zhang K, et al. Individualized surgical treatment for patients with tumours of the cervicothoracic junction. Interact Cardiovasc Thorac Surg 2022;34:1024-30. [Crossref] [PubMed]
- Azenha LF, Deckarm R, Minervini F, et al. Robotic vs. Transsternal Thymectomy: A Single Center Experience over 10 Years. J Clin Med 2021;10:4991. [Crossref] [PubMed]
- Daoud D, Darwish B, Zahra S, et al. Giant thymoma presenting as a large bilateral intrathoracic mass: A case report and a comparison between median sternotomy and hemiclamshell approach. Ann Med Surg (Lond) 2021;70:102859. [Crossref] [PubMed]
- Fanti S, Farsad M, Battista G, et al. Somatostatin receptor scintigraphy for bronchial carcinoid follow-up. Clin Nucl Med 2003;28:548-52. [Crossref] [PubMed]
- Pelosi G, Petrella F, Sandri MT, et al. A primary pure yolk sac tumor of the lung exhibiting CDX-2 immunoreactivity and increased serum levels of alkaline phosphatase intestinal isoenzyme. Int J Surg Pathol 2006;14:247-51. [Crossref] [PubMed]
- Sakakura N, Nakai A, Suda H, et al. Life-threatening massive bleeding in the pulmonary trunk adjacent to the right ventricular outflow tract during the resection of a large mediastinal germ cell tumor: proposed safety measures in the absence of cardiovascular surgeons: a case report. Mediastinum 2021;5:19. [Crossref] [PubMed]
- Fujiwara A, Funaki S, Ose N, et al. Surgical resection for advanced thymic malignancy with pulmonary hilar invasion using hemi-clamshell approach. J Thorac Dis 2018;10:6475-81. [Crossref] [PubMed]
Cite this article as: Petrella F, Rizzo SMR. The hemiclamshell approach to bulky cervico-mediastinal lesions: how to do it. Mediastinum 2024;8:9.



