
Anatomy of mediastinal veins and nerves
Introduction
The mediastinum is frequently encountered by thoracic surgeons for both benign and malignant disease. As part of a special series on the mediastinum, this article is meant to serve as a brief review of mediastinal anatomy and supplement the other articles within the series. This manuscript focuses on the surgical anatomy of the mediastinal veins and nerves and reviews surface landmarks for vein connections. The mediastinum is generally understood as four anatomical compartments.
Superior mediastinum
The borders of the superior mediastinum include the thoracic aperture superiorly, the angle of Louis anteriorly, and the T4/T5 vertebral bodies posteriorly. The superior mediastinal contents include the thymus gland and great vessels, including the right and left brachiocephalic vein and the confluence of the internal jugular vein with each of these structures. It is through the superior mediastinum that the vagus, recurrent laryngeal and phrenic nerves descend into the mediastinum.
The superior mediastinum also accommodates the trachea and esophagus. As such, tumors and cysts in the anterior mediastinum can cause compression or invasion of surrounding venous and nerve structures (1-3).
From a surgical perspective, the superior mediastinum can be approached via cervical or anterior mediastinoscopy, as for lymph node sampling in lung cancer. It can also be approached from median sternotomy or from a lateral decubitus video assisted thoracic surgery (VATS) or thoracotomy, as for thymectomy.
During cervical mediastinoscopy, a mediastinoscope is inserted under the pretracheal fascia and along the anterior surface of the trachea. One major landmark for mediastinoscopy is the left brachiocephalic artery, which can be palpated anterior to the pretracheal fascia. The left brachiocephalic vein travels superficial to the artery, just behind the sternum. The internal jugular and subclavian veins meet posterior to the sternoclavicular (SC) joints to form the bilateral brachiocephalic veins. Importantly, the left brachiocephalic vein is 2 cm longer than the right, because it passes over the arch of the aorta to enter into the right sided superior vena cava (SVC). In turn, the brachiocephalic veins combine to form the SVC. At the right tracheobronchial angle, the azygous vein travels from posterior to anterior to drain into the SVC. The azygous vein from the mediastinoscope appears as a faint blue or green structure within the mediastinal fat just to the right of the takeoff of the right mainstem bronchus (4).
The SVC terminates in the middle mediastinum and joins the right atrium. The SVC forms the posterior boundary of the transverse pericardial sinus.
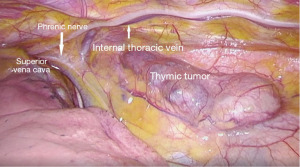
Approached from a median sternotomy, the most superficial structure to be encountered is the thymus gland. While the gland typically recedes in early adulthood, there are varying levels of remnant thymus gland in adults, and thymic masses can obtain size enough to account for compression of nearby structures. The veins of the thymus gland typically drain into the left brachiocephalic, the left internal thoracic, or the inferior thyroid veins. Approached via VATS for thymectomy (Figure 1), the junction of the left brachiocephalic vein and the SVC forms a useful landmark (4).
The vagus nerve leaves the skull and descends the neck posterior and lateral to the carotid arteries in the carotid sheath. Each nerve travels into the superior mediastinum posterior to the associated SC joint and brachiocephalic vein. The right vagus nerve enters the chest anterior to the right subclavian artery, where it gives off the right recurrent laryngeal nerve. The nerve then hooks behind the subclavian artery and ascends in the tracheoesophageal groove where it innervates the larynx. The right vagus nerve continues on behind the right brachiocephalic vein and branches into the right pulmonary plexus and right esophageal plexus. The left vagus nerve travels within the neck posterior to the common carotid artery. It then enters the mediastinum between the left common carotid and the subclavian arteries. At the left side of the aortic arch, it travels posteriorly behind the left phrenic nerve. It is separated from the left phrenic nerve by the left superior intercostal vein. The left vagus nerve then passes medially, where along the inferior aspect of the arch, it gives off the left recurrent laryngeal nerve, immediately lateral to the ligamentum arteriosum. The left vagus nerve travels inferiorly and gives fibers to the pulmonary and esophageal plexi.
The phrenic nerve originates from the C3, C4 and C5 nerve roots bilaterally and supplies the sensory and nerve fibers to the diaphragm. The phrenic nerve also supplies sensory fibers to the pericardium and mediastinal pleura. It enters the chest anterior to the subclavian artery. The left phrenic nerve frequently lies medial to the internal thoracic artery, and as such the left phrenic nerve is more susceptible to injury during sternotomy or thymectomy. Both phrenic nerves pass anterior to their respective pulmonary hila. The right phrenic nerve passes on the right side of the inferior vena cava (IVC), where it penetrates the diaphragm muscle near the caval aperture. The left phrenic nerve passes between the subclavian and common carotid arteries, crosses the medial surface of the arch of the aorta, and descends superficially along the pericardium. It then penetrates the diaphragm lateral to the heart. Additional branching of the phrenic nerve happens on the abdominal surface of the diaphragm.
Anterior mediastinum
The anterior mediastinum is the smallest subdivision and lies between the body of the sternum (below the angle of Louis) and the pericardium. It consists of mostly fat, a few lymph nodes, loose connective tissue and branches of the internal thoracic vessels.
Middle mediastinum
The middle mediastinum is bordered by the pericardium anteriorly and posteriorly, the lungs laterally, the diaphragm inferiorly, and terminates superiorly at the level of the angle of Louis. It contains the heart, great vessel roots, as well as the trachea and main bronchi.
The trachea ranges from 10–13 cm in length and divides into the right and left mainstem bronchi at the carina behind the angle of Louis (5). The mainstem bronchi then join the left and right lung hila at the T6 and T4 levels, respectively.
Surface landmarks for the junction of the mediastinal veins will be discussed in a later section. The internal jugular and subclavian veins converge bilaterally into the brachiocephalic veins which then merge into the SVC. The IVC enters the chest through the diaphragm at T8 and joins the right atrium at the level of the sixth costal cartilage.
As mentioned previously, both phrenic nerves traverse the middle mediastinum before entering the diaphragm. The left phrenic nerve passes through the middle mediastinum over the left ventricle while the right phrenic descends to the right of the SVC, right heart border, and IVC. Both phrenic nerves then penetrate the diaphragm. The two vagus nerves run posteriorly to the mainstem bronchi, eventually branching into or contributing to the pulmonary and esophageal plexi. The cardiac plexus is additionally present within the middle mediastinum.
Posterior mediastinum
The posterior mediastinum is located inferior to the angle of Louis, anterior to the T5-T1 vertebrae, posterior to the left atrium, pericardium and diaphragm and between the parietal pleura of the lungs. It contains the thoracic aorta, the thoracic duct and lymphatics, posterior mediastinal lymph nodes, the azygous and hemiazygous veins. The thoracic sympathetic trunk lies lateral to the vertebral bodies and is often referred to as a posterior mediastinal structure.
The azygous veins lie lateral to the vertebral column and drain the back and thoracoabdominal walls as well as the mediastinal viscera. There is great anatomic variation in the course and caliber of these veins and their tributaries. The azygous and the hemiazygous vein usually arise posteriorly from the IVC or inferior renal vein.
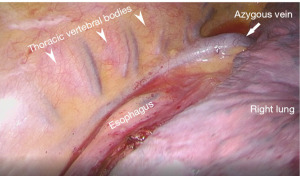
The azygous vein establishes a collateral pathway between the IVC and SVC and drains the posterior chest wall and abdomen. Figure 2 demonstrates the azygous vein as seen in the posterior mediastinum via a VATS approach to esophagectomy. It ascends through the posterior mediastinum, passing close to the right side of the bodies of the inferior 8 thoracic vertebral bodies. It travels over the esophagus, trachea, and right hilum to the SVC.
The hemiazygous vein arises by the junction of the left subcostal and ascending lumbar veins. It ascends laterally and to the left of the thoracic vertebral bodies and posterior to the aorta. It then crosses to the right side at the level of T9, posterior to the aorta and esophagus, to join the azygous vein.
The splanchnic nerves and the sympathetic trunks make up the bulk of the nerves in the posterior mediastinum. The sympathetic trunks comprise a large part of the autonomic nervous system. The thoracic trunks are in continuity with the cervical and lumbar trunks. The thoracic trunks lie in positions relative to their position in the thorax. They lie on the head of the ribs in the superior chest, the costovertebral joints in the mid chest and the vertebral bodies in the inferior chest. The lower thoracic splanchnic nerves supply fibers below the diaphragm. They consist of pre-synaptic fibers of the 5th–12th sympathetic ganglia, which pass through the diaphragm to supply the abdominal viscera.
Surface landmarks for vein connections
In addition to understanding the relation of the mediastinal structures to each other, knowledge of surface markers for venous junctions proves useful in mediastinal surgery. The medial border of the sternocleidomastoid serves as a useful marker for the internal jugular vein. The internal jugular and subclavian veins merge to form the brachiocephalic veins behind the SC joints. The left brachiocephalic vein then crosses behind the manubrium to join the right brachiocephalic vein at the level of the first costal cartilage to form the SVC (6). To give an idea of the small space where these large veins combine, the average width of the manubrium is 4.9 cm in women and 5.7 cm in men (7). The azygous vein drains into the SVC at the level of the 2nd costal cartilage and the SVC joins the right atrium one interspace down at the right 3rd costochondral junction. Given the close proximity of the azygous to the cavo-atrial junction, dissection of this area should be done carefully to preserve the azygous for reimplantation later in an SVC reconstruction. The IVC enters the right atrium behind the 6th costochondral junction.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Editorial Office, Mediastinum for the series “Venous Surgery of the Mediastinum”.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://med.amegroups.com/article/view/10.21037/med-20-65/coif). The series “Venous Surgery of the Mediastinum” was commissioned by the editorial office without any funding or sponsorship. ALD served as the unpaid Guest Editor of the series. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Moore KL, Dalley AF. Ch. 1, Thorax. In: Clinically Oriented Anatomy. 5th edition. Baltimore, MD, USA: Lippincott Williams & Wilkins, 2006:77-184.
- Sugarbaker DJ, Bueno R, Burt BM, et al. Ch. 156: Overview of Benign and Malignant Mediastinal Diseases. In: Adult Chest Surgery. 3rd edition. New York, NY, USA: McGraw-Hill Education, 2020:1368-74.
- Netter FH. Section 3, Thorax. In: Atlas of Human Anatomy. 5th edition. Philadelphia, PA, USA: Saunders, 2011:175-239.
- Scott-Conner CEH, DL. Ch. 20-21. In: Operative Anatomy. 3rd edition. Philadelphia, PA, USA: Lippincott Williams & Wilkins, 2011:152-63.
- Furlow PW, Mathisen DJ. Surgical anatomy of the trachea. Ann Cardiothorac Surg 2018;7:255-60. [Crossref] [PubMed]
- Sayeed RA, Darling GE. Surface anatomy and surface landmarks for thoracic surgery. Thorac Surg Clin 2007;17:449-61. v. [Crossref] [PubMed]
- Torwalt CR, Hoppa RD. A test of sex determination from measurements of chest radiographs. J Forensic Sci 2005;50:785-90. [Crossref] [PubMed]
Cite this article as: White A, Deeb AL. Anatomy of mediastinal veins and nerves. Mediastinum 2023;7:14.


