
Surgery for recurrent thymoma during the COVID-19 pandemic: a narrative review
Introduction
Surgical resection is the mainstay of treatment of thymoma and has been reported to be safe with improved survival even in those with stage III and IVa thymoma (1,2). Despite this, a number of patients who have undergone surgical resection may have recurrence of disease following resection. The most common site of recurrence is in the pleural cavity and is less common to recur in the anterior mediastinum, aside from cases where complete resection has not been achieved (3). However, recurrence has also been reported in those with initial complete R0 resection (4).
In one of the larger studies reported in the literature, one group demonstrated that good long term outcomes can be achieved in the case of complete resection of recurrent disease, with survival up to 82% at 5 years (4).
The SARS-Cov-2 (coronavirus disease 19; COVID-19) pandemic has caused significant mortality worldwide. Whilst the focus has been on reducing the number of infections by introducing isolation protocols for those with symptoms and for those who have tested positive for COVID-19, there remains a significant impact on the delivery of healthcare services in other specialities, such as in cancer care and cardiovascular disease (5). For example, in the case of lung cancer, there was a 40% reduction in the number of patients referred for urgent review for the investigation of possible lung cancer (6). This is likely to be driven by the seemingly appropriate advice to stay at home and isolate if one has symptoms of COVID-19 such as a continuous dry cough which of course may also be the presenting symptom of lung cancer.
In the United Kingdom, during the initial peak of the pandemic, and again during the second wave in late 2020, hospital wards have been cleared and many elective procedures and interventions have been postponed. Where possible, surgery and treatment for urgent conditions has continued. We have previously reported on our experience in management of lung cancer patients requiring surgery during the COVID-19 pandemic (7). During this period, we also continued to offer surgery to those with mediastinal tumours and indeed, patients with recurrent thymoma who have been shown to benefit from surgical resection.
Our aim was therefore to present our experience of patients operated on at a single centre in the UK for recurrent thymoma during the COVID-19 pandemic. We present the following article in accordance with the Narrative Review Reporting Checklist (available at: http://dx.doi.org/10.21037/med-21-10).
Patients and methods
A retrospective review of patients undergoing surgical resection by a single surgeon during the COVID-19 pandemic (from March 2020 to the present day) was performed. Seven thoracic surgeons cover 17 peripheral hospitals but only patients with recurrent thymoma or advanced thymoma discussed at the thymoma multidisciplinary meeting were included. All patients consented to be included in the case series. Patients had a preoperative computed tomography (CT) scan and a positron emission tomography (PET) scan. MRI scanning was performed when there was concern regarding invasion of the heart or great vessels. All patients had full lung function tests and echocardiogram as routine pre-operative work up. Patients were discussed at the local multidisciplinary meeting to determine suitability of surgical resection. The definition of recurrent disease was disease recurrence in the context of previous R0 resection.
Demographic and pathological data [age, presence of myasthenia gravis (MG), postoperative complications, pre and postoperative treatment, patterns of recurrence, and long-term follow-up information] were reviewed retrospectively.
All procedures were performed with radical intent. Prior to admission, patients were required to self isolate for, initially, 14 days prior to admission, however over time our unit protocols were modified and self isolation was required for 7 days prior to admission. All patients underwent screening for COVID-19 3 days before admission and were admitted only after returning a negative test. These patients were admitted on our unit’s ‘green’ pathway (‘amber’ being the pathway for those who cannot isolate and ‘red’ being for those with COVID-19). Upon admission, one day prior to surgery, patients underwent a repeat polymerase chain reaction (PCR) test, prior to surgery and would only proceed with surgery if this swab was negative. All patients are nursed in a single room and each patient is required to wear a surgical mask when entering shared or communal areas of the hospital.
Results
During COVID-19 pandemic between March 2020 and March 2021, three patients were operated for recurrent thymoma. Additionally, during the same period, 4 patients underwent surgery for stage III and IVa thymoma. For the purposes of the current study, the three patients undergoing surgery for recurrent thymoma were the subjects.
Patient characteristics are shown in Table 1. Patient 1, who presented with MG underwent median sternotomy thymectomy and wedge resection of the right upper lobe for a B2/B3 thymoma in January 2019, which was followed by chemotherapy. She presented one year following her initial surgery with pleural recurrence and she underwent right thoracotomy and partial pleurectomy in the lower right chest as well as wedge resection of the right lower lobe and resection and reconstruction of the diaphragm in May 2020, with complete macroscopic resection and clear resection margins. Diaphragmatic reconstruction was performed using a biological mesh (Surgimend®, Integra Lifesciences, New Jersey, USA) to reduce the risks of infection. Unfortunately, this patient has re-presented again with bilateral pleural recurrence for which she has undergone chemotherapy with partial response and is awaiting surgery for disease of the left hemithorax and radiotherapy of the right hemithorax.
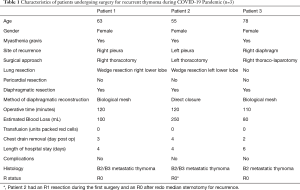
Full table
Patient 2 presented with symptoms of MG and underwent median sternotomy and debulking surgery for a B2 non-invasive thymoma in 2010, with R1 resection followed by radiotherapy. In 2012 the patient was found to have disease recurrence in the anterior mediastinum and so underwent redo sternotomy for thymoma recurrence. Resection was complete and the patient received radiotherapy postoperatively. She was noted in October 2020 to have a left basal pleural nodule which was positive on PET scanning. The patient underwent left thoracotomy and wedge resection of the upper and lower lobes, pleurectomy and diaphragmatic resection and reconstruction in November 2020, the pathology of which demonstrated a recurrent B2 thymoma with macroscopically complete resection. A CT scan performed in January 2021 did not show any residual disease.
Patient 3 underwent thymectomy for stage II thymoma in 2005, having presented with MG. In 2016, the patient was noted to have a right pleural nodule, which was positive on PET scanning. She therefore underwent right thoracotomy, resection of diaphragmatic nodules, diaphragmatic plication, resection of visceral pleural nodules and posterior parietal pleurectomy in October 2016. The pathology demonstrated recurrences of type B2 thymoma which were completely excised. The patient presented again in 2018 with a right sided paraspinal lesion, which was positive on PET scanning and underwent redo right thoracotomy and resection of this lesion and pleurectomy, however the pathology demonstrated no evidence of disease recurrence and the lesion was a reactive lymph node. She was noted on follow up scanning in November 2020 to have a new peri-diaphragmatic soft tissue mass, which demonstrated interval growth and so she underwent re-redo right thoracotomy and resection of the peri-diaphragmatic lesion and diaphragm resection and reconstruction with a biological patch in January 2021. The pathology of this lesion has shown a completely excised B2 thymoma metastasis.
All patients had a planned admission to the intensive care unit for one night for monitoring given the history of MG. There was no perioperative mortality in any of the patients operated during the COVID-19 pandemic. The duration of chest drainage was 3, 4 and 2 days respectively. Length of hospital stay was 4 days in the first 2 patients and 5 days in the third. There were no postoperative complications in any of these patients and no patients tested positive for COVID-19 in the postoperative period or were re admitted to hospital.
Discussion
Whilst relatively uncommon, we have demonstrated that surgery for recurrent thymoma can be performed with low perioperative mortality and with complete macroscopic resection in the majority of cases. Although our series is of a relatively small number of patients, we have demonstrated that the risks of perioperative COVID-19 infection are low, when patients are admitted through a managed pathway.
We have previously reported our experience of the surgical treatment of lung cancer during the COVID-19 pandemic (7). We believe that ensuring strict protocols in identifying those with COVID-19 are adhered to results in reduced risk of transmission to and from patients being admitted for elective surgery for cancer.
Much debate has ensued following the first wave of coronavirus infection in Spring of 2020, where the majority of elective services were halted or significantly reduced in capacity. As a result, there were a number of patients in whom treatment of non COVID related conditions was delayed or even cancelled. Initially, at the beginning of the pandemic, it was considered that there would be a relatively short impact on healthcare systems and as a result, a relatively short impact on the provision of healthcare for other important conditions. With the second wave of the pandemic, this may not necessarily be the case. In a study by Lai and colleagues, they have modelled that with the decline in urgent referrals for cancer care as well as other measures such as attendance at chemotherapy sessions, there are likely to be more than 17,000 excess deaths in 1 year, indirectly related to COVID-19 (8). Of course, patients with cancer are at increased risk of also being infected and developing COVID and so in these patients, the same group estimated 9,000 excess deaths in 1 year directly related to COVID in cancer patients (8).
Since September 2020, cases of COVID-19 have been rising significantly, and even with a second national lockdown in November of 2020, the UK healthcare service is under significant strain. Perhaps differently during this second wave of the pandemic, there has been a greater emphasis on the continuation of the delivery of routine healthcare and this means the healthcare system is under even more duress than during the first wave of the pandemic.
In our unit, to allow us to continue to offer as comprehensive a Thoracic Surgical service as possible, and to ensure we are able to continue to offer surgery, a number of protocols and practices have been established, as described in Methods.
Patients undergo PCR COVID-19 testing up to 72 hours prior to admission. Providing this test is negative, the patient is admitted the day before the planned surgery, where a second COVID-19 test is performed. Preoperative blood tests are performed and all patients have at least a chest X-ray performed. More recently, we have implemented a routine high-resolution CT scan in place of chest X-ray, performed on the day before surgery, to detect interstitial changes which may be related to COVID-19. Only if the patient is negative will they then undergo surgery. These patients are all nursed in areas separate to COVID patients in the pre and postoperative periods. In the operating theatre, full personal protective equipment (PPE), is worn by all members of the team, including FFP grade 3 mask, eye protection, gloves and gown. The patient is anesthetised and intubated inside the operating theatre, with as few team members present as possible. Surgery is performed without allowing admission of other staff into or out of the theatre until the operation is complete. All PPE is changed prior to receiving the next patient.
With these protocols, we have managed to continue to offer a full range of thoracic surgical treatments, such as surgery for recurrent thymoma, and since the beginning of the pandemic in March 2020, over 1,000 operations have been performed in our unit, of which 262 operations for benign (n=58) and malignant (n=204) disease have been performed by a single surgeon. There have been 9 postoperative COVID-19 infections and 3 deaths related to COVID. There were 3 patients readmitted with COVID-19 post discharge and are all alive. In the current cohort for recurrent thymoma, no patients were infected and developed COVID.
Regarding the patients undergoing surgery for recurrent thymoma, there are limited large studies reported. We have assessed the outcomes of surgery for recurrent thymoma compared to the most recently reported series, as shown in Table 2. The majority of patients undergoing surgery for recurrence will be those with pleural disease and these represent 75% of recurrences (10), as in the current series. It may be related to seeding during the initial surgery and a means of preventing this, particularly in those undergoing surgery via median sternotomy, would be to avoid breaching the mediastinal pleura. The diaphragm may be involved in these patients, as in all patients in the current series. Methods of diaphragmatic reconstruction include direct closure and the use of patches or mesh, which may or may not be absorbable. During the pandemic, we have opted for the use of biological meshes where diaphragmatic reconstruction is required. Whilst this may be a more costly, the use of prosthetic, non-absorbable material increases the risk of postoperative infection (11). Whilst the use of a biological mesh is unlikely to directly reduce the risk of COVID-19 infection, it will reduce the risk of postoperative infection which may require prolonged hospital admission or even readmission, with its risks of nosocomial COVID infection. The use of biological mesh for diaphragmatic reconstruction is now our preferred method of reconstruction.
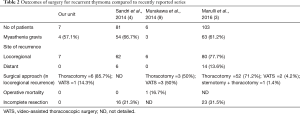
Full table
The optimal treatment of thymoma recurrence is not yet clearly defined given the relative lack of large studies. However, considering that the progression of recurrent disease is relatively slow, it would seem appropriate that repeat surgery for recurrence is justified. Despite this, multimodality treatment that combine radiotherapy and chemotherapy with surgery, are today widely accepted as treatment for recurrent thymoma. Therefore, given the improvement in survival and disease-free survival that have been observed (4), surgery for thymoma recurrence should continue to be advocated even during pandemic.
Conclusions
We have demonstrated that surgery for recurrent thymoma can be performed safely and complete macroscopic resection can be achieved. By ensuring adherence to strict infection control protocols, it is possible to offer surgery with low risk of perioperative COVID infection and related morbidity and mortality. Given the benefits seen in survival and disease-free survival, we believe surgery for recurrent thymoma should continue to be advocated even during the current viral pandemic.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Giuseppe Banna and Alfredo Addeo) for the series “Changes in management of mediastinal tumours following the surge of COVID-19 pandemic” published in Mediastinum. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review Reporting Checklist. Available at: http://dx.doi.org/10.21037/med-21-10
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at: http://dx.doi.org/10.21037/med-21-10). The series “Changes in management of mediastinal tumours following the surge of COVID-19 pandemic” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects for the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kumar A, Pulle MV, Asaf BB, et al. Surgical and Oncological Outcomes in Locally Advanced Thymoma. Indian J Surg Oncol 2020; [Crossref]
- Kanzaki R, Kanou T, Ose N, et al. Long-term outcomes of advanced thymoma in patients undergoing preoperative chemotherapy or chemoradiotherapy followed by surgery: A 20-year experience. Interact Cardiovasc Thorac Surg 2019;28:360-7. [Crossref] [PubMed]
- Marulli G, Margaritora S, Lucchi M, et al. Surgical treatment of recurrent thymoma: Is it worthwhile? Eur J Cardiothorac Surg 2016;49:327-32. [Crossref] [PubMed]
- Sandri A, Cusumano G, Lococo F, et al. Long-term results after treatment for recurrent thymoma a multicenter analysis. J Thorac Oncol 2014;9:1796-804. [Crossref] [PubMed]
- Ball S, Banerjee A, Berry C, et al. Monitoring indirect impact of COVID-19 pandemic on services for cardiovascular diseases in the UK. Heart 2020;106:1890-7. [Crossref] [PubMed]
- Greenwood E, Swanton C. Consequences of COVID-19 for cancer care — a CRUK perspective. Nat Rev Clin Oncol 2021;18:3-4. [Crossref] [PubMed]
- Bilkhu R, Billè A. Elective lung cancer surgery in the COVID-19 era: how do we do it? Tumori. 2020; [Epub ahead of print]. [Crossref] [PubMed]
- Lai AG, Pasea L, Banerjee A, et al. Estimated impact of the COVID-19 pandemic on cancer services and excess 1-year mortality in people with cancer and multimorbidity: near real-time data on cancer care, cancer deaths and a population-based cohort study. BMJ Open 2020;10:e043828 [Crossref] [PubMed]
- Murakawa T, Karasaki T, Kitano K, et al. Invasive thymoma disseminated into the pleural cavity: Mid-term results of surgical resection. Eur J Cardiothorac Surg 2015;47:567-72. [Crossref] [PubMed]
- Lucchi M, Mussi A. Surgical treatment of recurrent thymomas. J Thorac Oncol 2010;5:S348-51. [Crossref] [PubMed]
- Solli P, Bertolaccini L, Brandolini J, et al. Reconstructive techniques after diaphragm resection and use of the diaphragmatic flap in thoracic surgery. Shanghai Chest 2017;1:21. [Crossref]
Cite this article as: Bilkhu R, Billè A. Surgery for recurrent thymoma during the COVID-19 pandemic: a narrative review. Mediastinum 2021;5:17.


