
Bilateral diffuse pleural plaque with calcifications in pleural tuberculosis
Introduction
Tuberculosis (TB) remains one of the leading causes of deadliest infectious diseases in adults worldwide, resulting in approximately 1.5 million cases of deaths (1). Though pulmonary affection is a main presentation, pleural involvement is also another challenge in clinical practice, which accounts for 30–80% of all pleural effusions in developing countries (2). Typically, the TB pleural effusion is unilateral and manifests as a clear straw colored fluid (3); in rare cases, the pleural TB is in the form of plaque or thickening. In this case, the computed tomography (CT) scan suggests a bilateral pleural thickening with multiple pleural plaques, which could not be definitely diagnosed by biopsy. Finally, the patient was clinically diagnosed as pleural TB based on the effectiveness of anti-TB therapy. To improve the accuracy of diagnose and reduce the risk of transmission of this infectious disease, it’s necessary to report this unusual case.
Case presentation
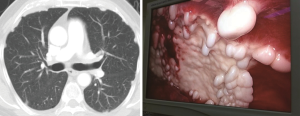
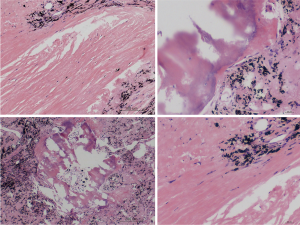
A 73-year-old man was admitted in hospital with repeated cough and right side pleural effusion for about 20 days. Repeated thoracentesis in local hospital revealed no significant result. No simultaneous phenomenon of polypnea, chest pain, tidal fever or night sweating was presented. He had hepatitis B for about 40 years and cirrhosis for 3 years without standard treatment. The patient had a history of heavy smoking and drinking and denied history of aerosols exposure, pulmonary TB and pleurisy. Thoracic CT showed bilateral pleural plaque with calcification (Figure 1). Laboratory examination revealed a serum low albumin, normal levels of serum creatinine, calcium and parathyroid hormone. Cultures of sputum revealed no evidence of cancer or TB. A pleural biopsy under thoracoscopy was performed and extensive pleural plaques were identified (Figure 1). Histopathology examination revealed no evidence of tumor or TB, but fibrosis and hyalinization as well as calcification, anthracosis and ossification (Figure 2). The patient presented persistent extensive pleural drainage (>800 mL/day) postoperatively until a diagnostical anti-TB treatment was introduced. After 1 week of anti-TB therapy, the volume of pleural drainage significantly decreased. A clinical diagnosis of pleural TB was thus confirmed and the anti-TB therapy was prescribed after hospital discharge.
Discussion
The manifestation of discrete pleural plaques in pleural TB has been reported in previous cases (4). Several new points could be drawn from our case. Firstly, pleural effusion usually occurs in the acute stage of TB while pleural thickening with calcification in longstanding lesion. The coexistence of two kinds of lesions at the same time in patients without history of TB was never reported. Secondly, all the previous cases reporting the discrete pleural plaques of pleural TB were unilateral, while the bilateral pleural involvement was not reported. Thirdly, to our knowledge, it is the first time that the image of pleural plaque with calcifications was directly seen by thoracoscopy.
In summary, pleural TB has a broad range of radiographic appearances and could manifest as other chest problems including malignancy. This case highlights the importance of diagnostical anti-TB treatment. The bilateral diffuse pleural calcifications could be an unusual manifestation of pleural TB.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/med.2018.04.01). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committees and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Zumla A, George A, Sharma V, et al. The WHO 2014 global tuberculosis report--further to go. Lancet Glob Health 2015;3:e10-2. [Crossref] [PubMed]
- Udwadia ZF, Sen T. Pleural tuberculosis: an update. Curr Opin Pulm Med 2010;16:399-406. [Crossref] [PubMed]
- Jolobe OM. Atypical tuberculous pleural effusions. Eur J Intern Med 2011;22:456-9. [Crossref] [PubMed]
- Atasoy C, Kaya A, Fitoz S, et al. Discrete pleural nodules associated with a parasternal mass: an unusual manifestation of tuberculosis. J Thorac Imaging 2002;17:74-7. [Crossref] [PubMed]
Cite this article as: Tie HT, Zhang M. Bilateral diffuse pleural plaque with calcifications in pleural tuberculosis. Mediastinum 2018;2:38.


