
A curious rarity of the thymus gland: the microscopic thymoma
In 1976, Rosai & Levine (1) opened a novel and interesting niche in the variegated field of the morphology of thymus gland in myasthenia gravis (MG). These authors firstly described a microscopic lesion having the histological features of a thymoma, occasionally observed in thymus gland removed during cardiac operations. They introduced the term “microscopic thymoma” to define these lesions histologically characterized by epithelial proliferation, smaller than 1mm in diameter, usually multifocal, sited in the cortex or medulla, in absence of a macroscopically evident thymic tumor (1-4). These lesions are observed in patients suffering from MG (5), an autoimmune disease that often shows several thymic abnormalities such as lymphoid follicular hyperplasia (15–85%) resulting from an abnormal activation of thymic B lymphocytes, or thymoma (10–25%), which originates from epithelial cells abnormally activated (6). Both features may coexist (7). In the remaining myasthenic patients the thymus appears involuted or normal.
Interestingly, according the 2004 WHO histological classification of the thymic epithelial tumor, these lesions are classified as A type thymoma. Indeed, hitherto 14 out of 18 cases already described belongs to type A thymoma (8), the remaining 4 reported by Vaideeswar et al. are not specified (3). This relationship is surprising because the A type tumor is not frequently associated with MG (9). The role of MG in the pathogenesis of the microscopic thymoma is not yet unveiled, particularly in the absence of lymphoid hyperplasia. Similarly, the pathogenesis and functional significance of microscopic thymoma of the thymic epithelium remains unclear. The rarity of the lesion does not favor the deepening of this essential issue.
Clinically, there are not evident symptoms referable to the lesion, whereas myasthenic signs and symptoms dominate the clinical scenario. Similarly, the imaging studies performed during the workup of the myasthenic disease did not allow the discovery of the lesions or thymic abnormalities.
The lack of morphological features of classic thymoma such as a lobulation and perivascular spaces as well as medullar differentiation and immature T-cells and the absence of data regarding the role in the development of the classic thymoma has suggested to define the microscopic thymoma as a nodular hyperplasia of the epithelium of the thymus (10,11). Hence, in the literature some author prefer to use the term of thymic nodular epithelial hyperplasia (3,12,13), but the latter would be a different pathologic entity according to Cheuk et al. (14).
The first clinical cases of microscopic thymoma were reported in 1992 by Pescarmona et al. 15 years after the first description, evidencing of the rarity of the pathology (15). These authors found multifocal microscopic thymomas in thymus of patients thymectomized for MG. The incidence of microscopic thymoma in autopsy specimens among myasthenic patients ranged between 4% and 15% in absence of clinical symptoms (15,16).
Fukuhara et al. (9) should be congratulated for their review focused on this niche of thymus morphology in myasthenic patients. We acknowledge the authors for having listed all cases reported in the literature since the very first description by Rosai and Levine (1). They have accurately collected the data from 18 patients outlining the clinical and morphological features described in each paper retrievable in the literature (9).
An evident homogeneity emerges within the analyzed cases. First of all, they result very infrequent. Apart from the 5 cases described by the authors themselves only another 13 were observed during a very long interval since the first three described by Pescarmona et al. in 1992 (15). All patients were myasthenic and they were all thymectomized. Nobody presented radiological signs at computed tomography. In the reported cases, a long lasting clinical improvement after thymectomy were observed (2,12,13,15). Most of them presented multifocal lesions (15,16) whilst solitary lesions may be considered sporadic.
Furthermore, respect to the other authors, Fukuhara et al. signaled the significant postoperative decrement of circulating anti-acetylcholine receptor antibodies thus demonstrating the advantages of extended thymectomy in reducing the antibodies (9).
Between 1986 and 2015 we performed more than 300 extended thymectomies through transsternal or video-assisted thoracoscopic (VATS) approaches for nonthymomatous MG. After having reviewed our series we found microscopic thymomas in 6 instances only and the features of these patients do not differ from those already described in literature as shown in Table 1.
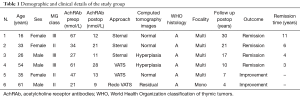
Full table
We incidentally discovered our first patient in occasion of a histological re-analysis performed for other reasons in 1996 within our own archival specimens of resected thymus for nonthymomatous MG. She was 16-year-old girl who in 1987 underwent a transsternal extended thymectomy for a IIB Osserman MG retrospectively judged as class III disease. The patient had an uneventful postoperative course and gradually achieved complete medication-free stable remission within 11 years from the procedure. She is still well without radiological evidence of the onset of a new thymoma at periodical controls.
Our sixth—at the moment last—case was detected in 2013 in a 61-year-old man class II myasthenic patient already operated 3 years before through a right-sided extended VATS thymectomy. This patient was reoperated through contralateral VATS given the persistence of the disease and the computed tomography image evidence of fat tissue residual in the aorto-pulmonary window. The histological examination revealed ectopic thymic tissue in the aorto-pulmonary mediastinal fat as well as a monofocal microscopic thymoma. After this second operation myasthenic symptoms had a progressive and significant improvement.
Finally, we would like also mention an adjunctive and more recent case of monofocal microscopic thymoma found in the neighboring tissue of a thymic cyst removed through VATS. In this case the patient had neither clinical symptoms nor electrophysiological sign and not even serological evidences of MG. Thus we did not include this case among of those listed in present publication.
According to our results we elaborated some hypothesis about the genesis of these tumors. Given the simultaneous occurrence of the lesions in both medullary and cortical compartments we agree with Pescarmona et al. who hypothesize a multifocal origin of microscopic thymoma from different epithelial clones hosted in different areas of the thymus (15). However, we also found these tumors freely growing in the mediastinal fat as a probable neoplastic evolution of ectopic thymic tissue.
Due to the rarity of the lesion it is difficult to predict the evolution of a microscopic thymoma. However, only the extensive removal of all perithymic fat tissue allows the detection and the elimination of all microscopic thymomas incidentally present. Furthermore these patients deserve a stricter regimen of follow up with yearly computed tomography in order to discover other lesions or thymic residual.
Extended thymectomy is has been already evoked to maximize the effect of thymectomy because of the elevate incidence of ectopic thymic tissue within the mediastinal fat (17-21). In our experience we observed an incidence of 80% (17,18) especially in pericardio-phrenic angle bilaterally, in aorto-caval groove and aorto-pulmonary window. The presence of multifocal microscopic thymoma is an additional reason to re-affirm that all thymic tissue, pericardial fat should be completely removed and many histological sections should be carefully examined.
The relationship between microscopic thymoma and MG are probable but obscure. Indeed, microscopic thymomas are discovered in thymuses resected in patients suffering with MG, but the genesis of MG, as well as clinical evolution and prognosis appear independent from the microscopic thymoma itself.
The benefit of thymectomy in myasthenic patients was highlighted by Blalock approximately 80 years ago (22). This author removed a cystic tumor of the thymus gland in a young woman who thereafter experienced the remission of the myasthenic symptoms (23). Recently, the randomized trial of thymectomy in MG (2) demonstrated that extended thymectomy improves clinical outcomes in non thymomatous MG. Although sternotomy allows the extended or maximal thymectomy both in non-thymomatous MG and thymomas, the persisting pain, the serious complications and the non cosmetic sequelae made this approach progressively less used. Thus, over the years, less invasive approaches have increasingly gained the preference of surgeons, patients and physicians. Less postoperative pain, reduced surgical trauma, better cosmesis and subsequent better postoperative quality of life had enhanced the use of minimally invasive approach. More recently, a subxiphoid single port thymectomy has been used to accomplish thymectomy (24). It is associated with lesser pain because there is no intercostal nerve damage and it permits an excellent cosmetic outcome (25) since only a single 3 cm abdominal skin incision is done.
Conclusions
Similarly to others, we conclude that the discovery of a microscopic thymoma may derive from an attentive microscopical and histological study of the areas including the thymic proliferation. The rarity of the lesion hinders both the morphological and clinical speculations. Further knowledge will probably occur during the coming years with the progressive accrual of new cases. According to this attainment a careful examination of all macroscopic non-neoplastic thymus resected as well as the analysis of the whole perithymic fat tissue in myasthenic patients becomes absolutely mandatory. Obviously, in order to facilitate the detection is necessary to perform many paraffin-embedded blocks of the surgically resected specimen.
To date, there is a certain data: microscopic thymoma is a rare, asymptomatic and occasionally discovered lesion that by the way necessitates of a better knowledge. On these bases the extended thymectomy becomes of pivotal importance.
Acknowledgments
We feel in debt with Dr. Gabriele Mazzitelli for his very precious and attentive cooperation in retrieving the sources of this review.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned and reviewed by Section Editor Dr. Zhuoqi Jia (Thoracic Department, the First Affiliated Hospital of Xi’an Jiaotong University, Xi’an, China).
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/med.2018.03.07). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Rosai J, Levine GD. Tumors of the thymus. In: Atlas of tumor pathology. 2nd series, fascicle 13. Washington, DC: Armed Forces Institute of Pathology, 1976.
- Wolfe GI, Kaminski HJ, Aban IB, et al. Randomized Trial of Thymectomy in Myasthenia Gravis. N Engl J Med 2016;375:511-22. [Crossref] [PubMed]
- Vaideeswar P. Microscopic thymoma: a report of four cases with review of literature. Indian J Pathol Microbiol 2011;54:539-41. [Crossref] [PubMed]
- Poulard G, Mosnier JF, Dumollard JM, et al. Microscopic thymoma and myasthenia gravis. Ann Pathol 1994;14:203-4. [PubMed]
- Mori T, Nomori H, Ikeda K, et al. Microscopic-sized "microthymoma" in patients with myasthenia gravis. Chest 2007;131:847-9. [Crossref] [PubMed]
- Travis WD, Brambilla E, Müller-Hermelink HK, et al. editors. Pathology and genetics of tumors of the lung, pleura, thymus and heart. Lyon: IARC Press, 2004;145-97.
- Drachman DB. Myasthenia gravis. N Engl J Med 1994;330:1797-810. [Crossref] [PubMed]
- Fukuhara M, Higuchi M, Owada Y, et al. Clinical and pathological aspects of microscopic thymoma with myasthenia gravis and review of published reports. J Thorac Dis 2017;9:1592-7. [Crossref] [PubMed]
- Rosai J. editor. Rosai and Ackerman’s Surgical Pathology. 8th ed. Edinburgh: Mosby, 2004: 459-514.
- Masaoka A, Monden Y, Nakahara K, et al. Follow-up study of thymomas with special reference to their clinical stages. Cancer 1981;48:2485-92. [Crossref] [PubMed]
- Engels EA, Pfeiffer RM. Malignant thymoma in the United States: demographic patterns in incidence and associations with subsequent malignancies. Int J Cancer 2003;105:546-51. [Crossref] [PubMed]
- Chalabreysse L, Orsini A, Vial C, et al. Microscopic thymoma. Interact Cardiovasc Thorac Surg 2007;6:133-5. [Crossref] [PubMed]
- Cornea R, Lazăr E, Dema A, et al. A nodular hyperplasia of the thymic epithelium (so-called microscopic thymoma). Rom J Morphol Embryol 2009;50:729-31. [PubMed]
- Cheuk W, Tsang WY, Chan JK. Microthymoma: definition of the entity and distinction from nodular hyperplasia of the thymic epithelium (so-called microscopic thymoma). Am J Surg Pathol 2005;29:415-9. [Crossref] [PubMed]
- Pescarmona E, Rosati S, Pisacane A, et al. Microscopic thymoma: histological evidence of multifocal cortical and medullary origin. Histopathology 1992;20:263-6. [Crossref] [PubMed]
- Puglisi F, Finato N, Mariuzzi L, et al. Microscopic thymoma and myasthenia gravis. J Clin Pathol 1995;48:682-3. [Crossref] [PubMed]
- Ambrogi V, Mineo TC. Active ectopic thymus predicts poor outcome after thymectomy in class III myasthenia gravis. J Thorac Cardiovasc Surg 2012;143:601-6. [Crossref] [PubMed]
- Mineo TC, Ambrogi V. Outcomes after thymectomy in class I myasthenia gravis. J Thorac Cardiovasc Surg 2013;145:1319-24. [Crossref] [PubMed]
- Jaretzki A 3rd, Penn AS, Younger DS, et al. “Maximal” thymectomy for myasthenia gravis. Results. J Thorac Cardiovasc Surg 1988;95:747-57. [PubMed]
- Fukai I, Funato Y, Mizuno T, et al. Distribution of thymic tissue in the mediastinal adipose tissue. J Thorac Cardiovasc Surg 1991;101:1099-102. [PubMed]
- Klimek-Piotrowska W, Mizia E, Kuzdzal J, et al. Ectopic thymic tissue in the mediastinum: limitations for the operative treatment of myasthenia gravis. Eur J Cardiothorac Surg 2012;42:61-5. [Crossref] [PubMed]
- Blalock A, Harvery AM, Ford FF, et al. The treatment of myasthenia gravis by removal of the thymus gland. JAMA 1941;117:1529-33. [Crossref]
- Blalock A, Mason MF, Morgan HJ, et al. Myasthenia gravis and tumors of the thymic region. Report of a case in which the tumor was removed. Ann Surg 1939;110:544-61. [Crossref] [PubMed]
- Suda T, Sugimura H, Tochii D, et al. Single-port thymectomy through an infrasternal approach. Ann Thorac Surg 2012;93:334-6. [Crossref] [PubMed]
- Yano M, Moriyama S, Haneda H, et al. The subxiphoid approach leads to less invasive thoracoscopic thymectomy than the lateral approach. World J Surg 2017;41:763-70. [Crossref] [PubMed]
Cite this article as: Mineo TC, Ambrogi V. A curious rarity of the thymus gland: the microscopic thymoma. Mediastinum 2018;2:16.


